- Record: found
- Abstract: found
- Article: found
Did the accuracy of oral amoxicillin dosing of children improve after British National Formulary dose revisions in 2014? National cross-sectional survey in England
Abstract
Objectives
Inaccurate antibiotic dosing can lead to treatment failure, fuel antimicrobial resistance and increase side effects. The British National Formulary for Children (BNFC) guidance recommends oral antibiotic dosing according to age bands as a proxy for weight. Recommended doses of amoxicillin for children were increased in 2014 ‘after widespread concerns of under dosing’. However, the impact of dose changes on British children of different weights is unknown, particularly given the rising prevalence of childhood obesity in the UK. We aimed to estimate the accuracy of oral amoxicillin dosing in British children before and after the revised BNFC guidance in 2014.
Setting and participants
We used data on age and weights for 1556 British children (aged 2–18 years) from a nationally representative cross-sectional survey, the Health Survey for England 2013.
Interventions
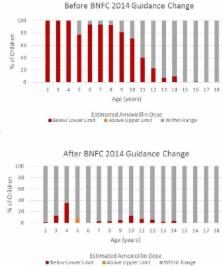
We calculated the doses each child would receive using the BNFC age band guidance, before and after the 2014 changes, against the ‘gold standard’ weight-based dose of amoxicillin, as per its summary of product characteristics.
Primary outcome measure
Assuming children of different weights were equally likely to receive antibiotics, we calculated the percentage of the children who would be at risk of misdosing by the BNFC age bands.
Results
Before 2014, 54.6% of children receiving oral amoxicillin would have been underdosed and no child would have received more than the recommended dose. After the BNFC guidance changed in 2014, the number of children estimated as underdosed dropped to 5.8%, but 0.5% of the children would have received too high a dose.
Related collections
Most cited references21
- Record: found
- Abstract: found
- Article: found
Maternal and child undernutrition and overweight in low-income and middle-income countries
- Record: found
- Abstract: found
- Article: not found
Undernutrition as an underlying cause of child deaths associated with diarrhea, pneumonia, malaria, and measles.

- Record: found
- Abstract: found
- Article: found