- Record: found
- Abstract: found
- Article: not found
WORKPLACE VIOLENCE AGAINST PHYSICIANS TREATING COVID-19 PATIENTS IN PERU: A CROSS-SECTIONAL STUDY

Read this article at
Abstract
Background
The COVID-19 pandemic is an unprecedented challenge to health systems that has revealed shortcomings and increased unmet demands. Such situations might exacerbate workplace violence (WPV) against doctors, as has been reported in several parts of the world.
Methods
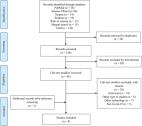
To identify the frequency and characteristics of WPV suffered by physicians attending COVID-19 patients in Peru, a descriptive, cross-sectional study was conducted with an online survey of 200 physicians.
Results
Of the survey respondents, 84.5% had suffered some type of violence 97.5% of these suffered non-physical violence. Suffering more than one incidence of violence was reported by 75.7% of respondents. The primary aggressor was a patient's family member or caregiver. Violence occurred most frequently in critical areas inside the health service facility, such as COVID-19 triage, tents, and hospital units, although it also occurred during teleconsultations. Multiple shortcomings of the health services were perceived as the main trigger of violence. Being a female physician (odds ratio [OR] = 2.8 [1.06–5.83]) and working in a COVID-19 ICU (OR = 5.84 [1.60–21.28]) were the main factors associated with WPV.
Related collections
Most cited references53

- Record: found
- Abstract: found
- Article: found
Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series
- Record: found
- Abstract: found
- Article: found
The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence
- Record: found
- Abstract: found
- Article: not found
