- Record: found
- Abstract: found
- Article: found
Single fraction radiosurgery/stereotactic body radiation therapy (SBRT) for spine metastasis: A dosimetric comparison of multiple delivery platforms
Read this article at
Abstract
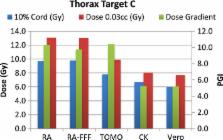
There are numerous commercial radiotherapy systems capable of delivering single fraction spine radiosurgery/ SBRT. We aim to compare the capabilities of several of these systems to deliver this treatment when following standardized criteria from a national protocol. Four distinct target lesions representing various case presentations of spine metastases were contoured in both the thoracic and lumbar spine of an anthropomorphic SBRT phantom. Single fraction radiosurgery/ SBRT plans were designed for each target with each of our treatment platforms. Plans were prescribed to 16 Gy in one fraction to cover 90% of the target volume using normal tissue and target constraints from RTOG 0631. We analyzed these plans with priority on the dose to 10% of the partial spinal cord and dose to 0.03 cc of the spinal cord. Each system was able to maintain 90% target coverage while meeting all the constraints of RTOG 0631. On average, CyberKnife was able to achieve the lowest spinal cord doses overall and also generated the sharpest dose falloff as indicated by the Paddick gradient index. Treatment times varied widely depending on the modality utilized. On average, treatment can be delivered faster with Flattening Filter Free RapidArc and Tomotherapy, compared to Vero and Cyberknife. While all systems analyzed were able to meet the dose constraints of RTOG 0631, unique characteristics of individual treatment modalities may guide modality selection. Specifically, certain modalities performed better than the others for specific target shapes and locations, and delivery time varied significantly among the different modalities. These findings could provide guidance in determining which of the available modalities would be preferable for the treatment of spine metastases based on individualized treatment goals.
Related collections
Most cited references11
- Record: found
- Abstract: found
- Article: not found
Randomized trial of short- versus long-course radiotherapy for palliation of painful bone metastases.
- Record: found
- Abstract: found
- Article: not found