- Record: found
- Abstract: found
- Article: found
Extrafine Beclometasone Dipropionate/Formoterol Fumarate vs Double Bronchodilation Therapy in Patients with COPD: A Historical Real-World Non-Inferiority Study
Abstract
Purpose
This study aimed to evaluate the non-inferiority of initiating extrafine beclometasone dipropionate/formoterol fumarate (BDP/FF) versus double bronchodilation (long-acting beta-agonists [LABA]/long-acting muscarinic antagonists [LAMA]) among patients with a history of chronic obstructive pulmonary disease (COPD) exacerbations.
Patients and Methods
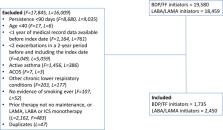
A historical cohort study was conducted using data from the UK’s Optimum Patient Care Research Database. Patients with COPD ≥40 years at diagnosis were included if they initiated extrafine BDP/FF or any LABA/LAMA double therapy as a step-up from no maintenance therapy or monotherapy with inhaled corticosteroids (ICS), LAMA, or LABA and a history of ≥2 moderate/severe exacerbations in the previous two years. The primary outcome was exacerbation rate from therapy initiation until a relevant therapy change or end of follow-up. Secondary outcomes included rate of acute respiratory events, acute oral corticosteroids (OCS) courses, and antibiotic prescriptions with lower respiratory indication, modified Medical Research Council score (mMRC) ≥2, and time to first pneumonia diagnosis. The non-inferiority boundary was set at a relative difference of 15% on the ratio scale. Five potential treatment effect modifiers were investigated.
Results
A total of 1735 patients initiated extrafine BDP/FF and 2450 patients initiated LABA/LAMA. The mean age was 70 years, 51% were male, 41% current smokers, and 85% had FEV 1 <80% predicted. Extrafine BDP/FF showed non-inferiority to LABA/LAMA for rate of exacerbations (incidence rate ratio [IRR] = 1.01 [95% CI 0.94–1.09]), acute respiratory events (IRR = 0.98 [0.92–1.04]), acute OCS courses (IRR = 1.01 [0.91–1.11]), and antibiotic prescriptions (IRR = 0.99 [0.90–1.09]), but not for mMRC (OR = 0.93 [0.69–1.27]) or risk of pneumonia (HR = 0.50 [0.14–1.73]). None of the a priori defined effect modifier candidates affected the comparative effectiveness.
Most cited references28
- Record: found
- Abstract: not found
- Book: not found
A simple sequentially rejective multiple test procedure
- Record: found
- Abstract: found
- Article: found
Once-Daily Single-Inhaler Triple versus Dual Therapy in Patients with COPD
- Record: found
- Abstract: found
- Article: not found