- Record: found
- Abstract: found
- Article: found
Multi-center evaluation of dose conformity in stereotactic body radiotherapy
Read this article at
Abstract
Background and purpose
Stereotactic body radiotherapy (SBRT) is an emerging technique for treating oligometastases, but limited data is available on what plan quality is achievable for a range of modalities and clinical sites.
Methods
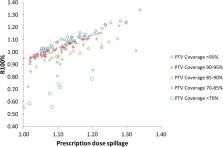
SBRT plans for lung, spine, bone, adrenal, liver and node sites from 17 participating centers were reviewed. Centers used various delivery techniques including static and rotational intensity-modulation and multiple non-coplanar beams. Plans were split into lung and other body sites and evaluated with different plan quality metrics, including two which are independent of target coverage; “prescription dose spillage” (PDS) and “modified gradient index” (MGI). These were compared to constraints from the ROSEL and RTOG 0813 clinical trials.
Results
Planning target volume (PTV) coverage was compromised (PTV V100% < 90%) in 29% of patient plans in order to meet organ-at-risk (OAR) tolerances, supporting the use of plan quality metrics which are independent of target coverage. Both lung (n = 48) and other body (n = 99) site PDS values agreed well with ROSEL constraints on dose spillage, but RTOG 0813 values were too high to detect sub-optimal plans. MGI values for lung plans were mis-matched to both sets of previous constraints, with ROSEL values too high and RTOG 0813 values too low. MGI values were lower for other body plans as expected, though this was only statistically significant for PTV volumes <20 cm 3.
Related collections
Most cited references32
- Record: found
- Abstract: found
- Article: not found
A conformation number to quantify the degree of conformality in brachytherapy and external beam irradiation: application to the prostate.
- Record: found
- Abstract: found
- Article: not found
A simple scoring ratio to index the conformity of radiosurgical treatment plans
- Record: found
- Abstract: found
- Article: not found