- Record: found
- Abstract: found
- Article: found
Effect of blastocyst shrinkage on assisted reproductive outcomes: a retrospective cohort study describing a new morphological evaluation of blastocyst pre-vitrification and post-warming
Read this article at
Abstract
Background
The failure of frozen-thawed blastocysts to re-expand adequately within a few hours after warming has been reported to have a negative impact on assisted reproductive technology (ART) outcomes. However, the extent to which this failure truly affects ART outcomes has not yet been presented in a manner that is easily understandable to medical practitioners and patients. This study aimed to assess the effects of blastocyst shrinkage on ART outcomes and determine a more effective morphological evaluation approach for use in clinical settings.
Methods
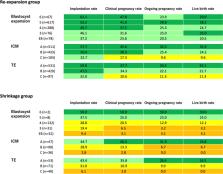
This retrospective observational cohort study of frozen-thawed blastocyst transfer cycles was conducted from April 2017 to March 2022. Overall, 1,331 cycles were eligible for inclusion, of which 999 were good-quality blastocysts (GQB) and 332 were non-good-quality blastocysts (non-GQB). All frozen-thawed blastocyst transfer cycles performed during the specified study period were included in the study. Exclusion criteria were established to mitigate potential sources of bias as these cycles could impact implantations. We calculated rates and age-adjusted odds ratios of implantation, clinical pregnancy, ongoing pregnancy, and live birth of the re-expansion group, which showed sufficient expansion, and shrinkage group, which showed insufficient expansion. We also calculated the implantation, clinical pregnancy, ongoing pregnancy, and live birth rates of the re-expansion and shrinkage groups for each morphological scoring system parameter.
Results
A reduced ART outcome was observed with use of blastocysts with shrinkage after vitrification/warming. The age-adjusted odds ratios for implantation, clinical pregnancy, ongoing pregnancy, and live birth were lower in the shrinkage group than in the re-expansion group.
Conclusions
This study examined the adverse effect of blastocyst shrinkage after warming and recovery culturing on reproductive outcomes in a clinically useful manner by retrospectively examining a substantial number of frozen-thawed embryo transfer cycles. The study findings can possibly reduce concerns regarding over- or under-estimation of blastocyst implantation by allowing providers and patients to refer to the data.
Related collections
Most cited references22
- Record: found
- Abstract: found
- Article: not found
Culture and transfer of human blastocysts.
- Record: found
- Abstract: not found
- Article: not found
Ice-free cryopreservation of mouse embryos at −196 °C by vitrification
- Record: found
- Abstract: found
- Article: not found