- Record: found
- Abstract: found
- Article: found
PERSISTENCE OF PLASMODIUM FALCIPARUM HRP2 ANTIGEN AFTER EFFECTIVE ANTIMALARIAL THERAPY
Read this article at
Abstract
Introduction:
Histidine Rich Protein 2 based (HRP2-based) malaria rapid diagnostic tests (mRDTs) have been shown to perform as well as routine light microscopy, however, they are limited by some factors including persistence of HRP2 antigenemia. In this paper we report the evaluation of an HRP2-based mRDT in a prospective study that enrolled children and followed them up for 28 days.
Methods:
Children aged below five years, with acute episode of fever/pyrexia, were enrolled. The enrolled participants had expert malaria microscopy and RDT done at enrolment (Day 0), and on days 1, 2, 3, 7, 14, 21, and 28. The malaria RDT test was considered positive when the antigen and control lines were visible in their respective windows, negative when only the control band was visible and invalid when the control band was not visible. Faint test lines were considered positive. The RDT results were compared to those of expert microscopy.
Results:
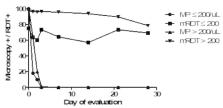
Two hundred and twenty-six children aged 29.2 ± 15.5 months were enrolled. The proportion of children positive by expert malaria microscopy and RDT was 100% and 95.6% respectively. During the 28 day follow up of the children the proportions positive by microscopy and RDT on days 3, 7, 14, and 28 were 1% and 94.6%, 0% and 93.5%, 0% and 91%, and 16.5% and 80.6% respectively. Gender and age dependent analysis of proportion of positive children were similar. Proportion of children with persistence of HRP2 antigen appeared to be lower in those with parasite density below 200/µL, however, this observation requires further evaluation in larger studies.
Related collections
Most cited references26
- Record: found
- Abstract: found
- Article: not found
A review of malaria diagnostic tools: microscopy and rapid diagnostic test (RDT).

- Record: found
- Abstract: found
- Article: found
Improving community health worker use of malaria rapid diagnostic tests in Zambia: package instructions, job aid and job aid-plus-training
- Record: found
- Abstract: found
- Article: not found