- Record: found
- Abstract: found
- Article: found
Analysis of Severe Illness After Postvaccination COVID-19 Breakthrough Among Adults With and Without HIV in the US
Read this article at
Key Points
Question
In 2021, among fully vaccinated people with breakthrough COVID-19 illness, was the risk of severe illness higher for people with HIV (PWH) compared with people without HIV (PWoH)?
Findings
In this cohort study of 3649 patients with breakthrough COVID-19, there was no overall difference in risk of severe disease between PWH and PWoH. PWH with CD4 cell count less than 350 cells/μL had a 59% increased risk of severe breakthrough illness compared with PWoH.
Meaning
Although vaccinations effectively reduce the risk of severe COVID-19 illness in both PWH and PWoH, these findings suggest that PWH with moderate or severe immune suppression (CD4 cell count <350 cells/μL) could be at higher risk of severe breakthrough infection compared with PWoH, and PWH with moderate immune suppression should be considered for additional vaccine dosages and other risk-reduction measures.
Abstract
This cohort study estimates the rate and risk of severe breakthrough COVID-19 illness among vaccinated people with HIV and people without HIV who experience a breakthrough infection.
Abstract
Importance
Understanding the severity of postvaccination SARS-CoV-2 (ie, COVID-19) breakthrough illness among people with HIV (PWH) can inform vaccine guidelines and risk-reduction recommendations.
Objective
To estimate the rate and risk of severe breakthrough illness among vaccinated PWH and people without HIV (PWoH) who experience a breakthrough infection.
Design, Setting, and Participants
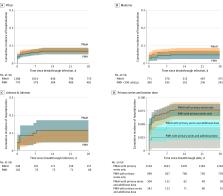
In this cohort study, the Corona-Infectious-Virus Epidemiology Team (CIVET-II) collaboration included adults (aged ≥18 years) with HIV who were receiving care and were fully vaccinated by June 30, 2021, along with PWoH matched according to date fully vaccinated, age group, race, ethnicity, and sex from 4 US integrated health systems and academic centers. Those with postvaccination COVID-19 breakthrough before December 31, 2021, were eligible.
Main Outcomes and Measures
The main outcome was severe COVID-19 breakthrough illness, defined as hospitalization within 28 days after a breakthrough SARS-CoV-2 infection with a primary or secondary COVID-19 discharge diagnosis. Discrete time proportional hazards models estimated adjusted hazard ratios (aHRs) and 95% CIs of severe breakthrough illness within 28 days of breakthrough COVID-19 by HIV status adjusting for demographic variables, COVID-19 vaccine type, and clinical factors. The proportion of patients who received mechanical ventilation or died was compared by HIV status.
Results
Among 3649 patients with breakthrough COVID-19 (1241 PWH and 2408 PWoH), most were aged 55 years or older (2182 patients [59.8%]) and male (3244 patients [88.9%]). The cumulative incidence of severe illness in the first 28 days was low and comparable between PWoH and PWH (7.3% vs 6.7%; risk difference, −0.67%; 95% CI, −2.58% to 1.23%). The risk of severe breakthrough illness was 59% higher in PWH with CD4 cell counts less than 350 cells/μL compared with PWoH (aHR, 1.59; 95% CI, 0.99 to 2.46; P = .049). In multivariable analyses among PWH, being female, older, having a cancer diagnosis, and lower CD4 cell count were associated with increased risk of severe breakthrough illness, whereas previous COVID-19 was associated with reduced risk. Among 249 hospitalized patients, 24 (9.6%) were mechanically ventilated and 20 (8.0%) died, with no difference by HIV status.
Conclusions and Relevance
In this cohort study, the risk of severe COVID-19 breakthrough illness within 28 days of a breakthrough infection was low among vaccinated PWH and PWoH. PWH with moderate or severe immune suppression had a higher risk of severe breakthrough infection and should be included in groups prioritized for additional vaccine doses and risk-reduction strategies.
Related collections
Most cited references38
- Record: found
- Abstract: found
- Article: not found
Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine
- Record: found
- Abstract: found
- Article: not found
Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine
- Record: found
- Abstract: found
- Article: not found