- Record: found
- Abstract: found
- Article: found
Recognizing Depression from the Microbiota–Gut–Brain Axis
Read this article at
Abstract
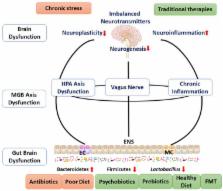
Major depression is one of the leading causes of disability, morbidity, and mortality worldwide. The brain–gut axis functions are disturbed, revealed by a dysfunction of the brain, immune system, endocrine system, and gut. Traditional depression treatments all target the brain, with different drugs and/or psychotherapy. Unfortunately, most of the patients have never received any treatment. Studies indicate that gut microbiota could be a direct cause for the disorder. Abnormal microbiota and the microbiota–gut–brain dysfunction may cause mental disorders, while correcting these disturbance could alleviate depression. Nowadays, the gut microbiota modulation has become a hot topic in treatment research of mental disorders. Depression is closely related with the health condition of the brain–gut axis, and maintaining/restoring the normal condition of gut microbiota helps in the prevention/therapy of mental disorders.
Related collections
Most cited references107
- Record: found
- Abstract: not found
- Article: not found
Major depressive disorder.
- Record: found
- Abstract: not found
- Article: not found
Mental health: a world of depression.
- Record: found
- Abstract: found
- Article: not found