- Record: found
- Abstract: found
- Article: found
Association between metabolic syndrome and endometrial cancer risk: a systematic review and meta-analysis of observational studies
Read this article at
Abstract
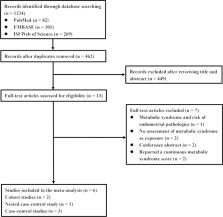
Existing evidence has revealed inconsistent results on the association between metabolic syndrome (MetS) and endometrial cancer (EC) risk. Herein, we aim to better understand this association. Systematic searches of PubMed, EMBASE, and Web of Science through 12 December 2019 were conducted. Observational studies that provided risk estimates of MetS and EC risk were eligible. The quality of the included studies was judged based on the Newcastle–Ottawa scale. Summary odds ratios (ORs) and 95% confidence intervals (CIs) were calculated using a random-effects model. Six studies, comprising 17,772 EC cases and 150,371 participants were included. MetS, diagnosed according to the criteria of the National Cholesterol Education Program—Third Adult Treatment Panel, was associated with an increased risk of EC (OR: 1.62; 95% CI = 1.26–2.07) with substantial heterogeneity (I 2 = 78.3%). Furthermore, we found that women with MetS, diagnosed according to the criteria of the International Diabetes Federation, had a significantly higher risk of EC compared to healthy controls (OR: 1.45; 95% CI = 1.16–1.81; I 2 = 64.6%). Our findings were generally consistent with the main results in the majority of prespecified subgroups, as well as in sensitivity analyses. In conclusion, MetS is associated with EC risk.
Related collections
Most cited references29
- Record: found
- Abstract: found
- Article: not found
Long-term all-cause mortality in cancer patients with preexisting diabetes mellitus: a systematic review and meta-analysis.
- Record: found
- Abstract: found
- Article: not found
Type I and II endometrial cancers: have they different risk factors?
- Record: found
- Abstract: found
- Article: not found