- Record: found
- Abstract: found
- Article: found
Meningo-cortical manifestations of myelin oligodendrocyte glycoprotein antibody-associated disease: Review of a novel clinico-radiographic spectrum
Read this article at
Abstract
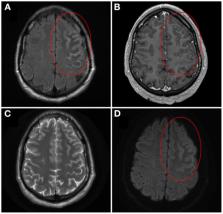
Myelin oligodendrocyte glycoprotein antibody-associated disease (MOGAD) is an inflammatory demyelinating disease that is distinct from multiple sclerosis. Initial manifestations of MOGAD that were reported in the literature included optic neuritis, myelitis, brainstem demyelination and encephalitis, with emphasis placed on acute disseminated encephalomyelitis (ADEM) as the primary encephalitic presentation. In 2017, however, Ogawa et al. described four patients with seizures, unilateral cortical hyperintensities on brain magnetic resonance imaging T2-fluid-attenuated inversion recovery sequences, and anti-MOG positivity, indicating a potentially novel form of encephalitis in MOGAD. In 2019, we systematically reviewed the literature to better characterize this unique syndrome, which we referred to as unilateral cortical FLAIR-hyperintense Lesions in Anti-MOG-associated Encephalitis with Seizures (FLAMES). Subsequently, anti-MOG positivity in patients with a variety of cortical and meningeal disease presentations has been reported, indicating a broader spectrum of meningo-cortical manifestations in MOGAD that we review herein.
Related collections
Most cited references61
- Record: found
- Abstract: found
- Article: not found
A clinical approach to diagnosis of autoimmune encephalitis.
- Record: found
- Abstract: found
- Article: not found
Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study.
- Record: found
- Abstract: found
- Article: not found