- Record: found
- Abstract: found
- Article: not found
Evaluation of the risk factors associated with conversion of intended deep anterior lamellar keratoplasty to penetrating keratoplasty
Abstract
Background/aims
To identify and evaluate risk factors associated with the need to convert intended deep anterior lamellar keratoplasty (DALK) to penetrating keratoplasty (PK).
Methods
Retrospective institutional cohort study including all consecutive eyes undergoing intended DALK between May 2015 and October 2018 at ‘Villa Igea’ Hospital (Forli, Italy). The indications for surgery were categorised as (1) keratoconus without scarring; (2) keratoconus with scarring; (3) non-keratoconus without scarring; and (4) non-keratoconus with scarring. Multivariate binary logistic regression analysis was performed, introducing, as independent variables, those that reached a significance level of less than 0.05 in univariate analysis. The main outcome measure was whether or not conversion to a PK occurred.
Results
705 eyes were included, with conversion to PK occurring in 16.2% (n=114) of cases. The factors that remained significant in multivariate analysis were corneal scarring (OR=3.52, p<0.001), manual dissection (OR=42.66, p<0.001), type 2 bubble (OR=90.65, p<0.001) and surgeon inexperience (OR=10.86, p<0.001). A receiver operating characteristic (ROC) curve based on the factors significant in the multivariate binary logistic regression analysis achieved a sensitivity of 89.5% (95% CI 82.3% to 94.4%) and a specificity of 80.2% (95% CI 76.8% to 83.3%) with an area under the ROC curve of 0.91 (95% CI 0.88 to 0.93) (p<0.001)
Conclusion
Occurrence of a type 2 bubble, the need for manual dissection, the presence of scarring and surgeon inexperience are independent risk factors for the need to convert intended DALK to PK. Correct identification and management of the type of bubble achieved during pneumatic dissection is instrumental in minimising the rate of conversion to PK.
Related collections
Most cited references14
- Record: found
- Abstract: not found
- Article: not found
Big-bubble technique to bare descemet’s membrane in anterior lamellar keratoplasty
- Record: found
- Abstract: not found
- Article: not found
Deep Anterior Lamellar Keratoplasty for Keratoconus: Multisurgeon Results
- Record: found
- Abstract: found
- Article: found
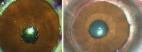
Differentiating type 1 from type 2 big bubbles in deep anterior lamellar keratoplasty
Author and article information
Comments
Comment on this article
Similar content949
- Endophthalmitis by Pseudomonas aeruginosa. after penetrating keratoplasty, case report with an epidemiological investigation Translated title: Endoftalmitis por Pseudomonas aeruginosa posterior a queratoplastia penetrante, reporte de caso con investigación epidemiológicaAuthors: Claudia Blanco, María X Núñez