- Record: found
- Abstract: found
- Article: found
Pathogenic Mechanisms Associated With Different Clinical Courses of Multiple Sclerosis
Read this article at
Abstract
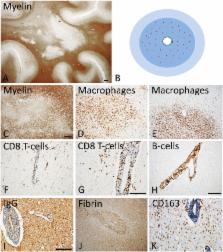
In the majority of patients multiple sclerosis starts with a relapsing remitting course (RRMS), which may at later times transform into secondary progressive disease (SPMS). In a minority of patients the relapsing remitting disease is skipped and the patients show progression from the onset (primary progressive MS, PPMS). Evidence obtained so far indicate major differences between RRMS and progressive MS, but no essential differences between SPMS and PPMS, with the exception of a lower incidence in the global load of focal white matter lesions and in particular in the presence of classical active plaques in PPMS. We suggest that in MS patients two types of inflammation occur, which develop in parallel but partially independent from each other. The first is the focal bulk invasion of T- and B-lymphocytes with profound blood brain barrier leakage, which predominately affects the white matter, and which gives rise to classical active demyelinated plaques. The other type of inflammation is a slow accumulation of T-cells and B-cells in the absence of major blood brain barrier damage in the connective tissue spaces of the brain, such as the meninges and the large perivascular Virchow Robin spaces, where they may form aggregates or in most severe cases structures in part resembling tertiary lymph follicles. This type of inflammation is associated with the formation of subpial demyelinated lesions in the cerebral and cerebellar cortex, with slow expansion of pre-existing lesions in the white matter and with diffuse neurodegeneration in the normal appearing white or gray matter. The first type of inflammation dominates in acute and relapsing MS. The second type of inflammation is already present in early stages of MS, but gradually increases with disease duration and patient age. It is suggested that CD8 + T-lymphocytes remain in the brain and spinal cord as tissue resident cells, which may focally propagate neuroinflammation, when they re-encounter their cognate antigen. B-lymphocytes may propagate demyelination and neurodegeneration, most likely by producing soluble neurotoxic factors. Whether lymphocytes within the brain tissue of MS lesions have also regulatory functions is presently unknown. Key open questions in MS research are the identification of the target antigen recognized by tissue resident CD8 + T-cells and B-cells and the molecular nature of the soluble inflammatory mediators, which may trigger tissue damage.
Related collections
Most cited references83

- Record: found
- Abstract: found
- Article: found
The relation between inflammation and neurodegeneration in multiple sclerosis brains
- Record: found
- Abstract: found
- Article: not found
Meningeal B-cell follicles in secondary progressive multiple sclerosis associate with early onset of disease and severe cortical pathology.
- Record: found
- Abstract: found
- Article: not found