- Record: found
- Abstract: found
- Article: found
Association of Social and Demographic Factors With COVID-19 Incidence and Death Rates in the US
Read this article at
Key Points
Question
Are population-level social factors associated with coronavirus disease 2019 (COVID-19) incidence and mortality?
Abstract
This cross-sectional study examines the county-level associations of sociodemographic risk factors with coronavirus disease 2019 incidence and mortality in the US.
Abstract
Importance
Descriptive data have revealed significant racial/ethnic disparities in coronavirus disease 2019 (COVID-19) cases in the US, but underlying mechanisms of disparities remain unknown.
Objective
To examine the association between county-level sociodemographic risk factors and US COVID-19 incidence and mortality.
Design, Setting, and Participants
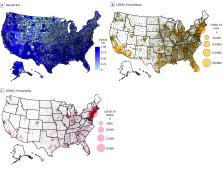
This cross-sectional study analyzed the association between US county-level sociodemographic risk factors and COVID-19 incidence using mixed-effects negative binomial regression, and COVID-19 mortality using zero-inflated negative binomial regression. Data on COVID-19 incidence and mortality were collected from January 20 to July 29, 2020. The association of social risk factors with weekly cumulative incidence and mortality was also examined by interacting time with the index measures, using a random intercept to account for repeated measures.
Main Outcomes and Measures
Sociodemographic data from publicly available data sets, including the US Centers for Disease Control and Prevention’s Social Vulnerability Index (SVI), which includes subindices of socioeconomic status, household composition and disability, racial/ethnic minority and English language proficiency status, and housing and transportation.
Results
As of July 29, 2020, there were a total of 4 289 283 COVID-19 cases and 147 074 COVID-19 deaths in the US. An increase of 0.1 point in SVI score was associated with a 14.3% increase in incidence rate (incidence rate ratio [IRR], 1.14; 95% CI, 1.13-1.16; P < .001) and 13.7% increase in mortality rate (IRR, 1.14; 95% CI, 1.12-1.16; P < .001), or an excess of 87 COVID-19 cases and 3 COVID-19 deaths per 100 000 population for a SVI score change from 0.5 to 0.6 in a midsize metropolitan county; subindices were also associated with both outcomes. A 0.1-point increase in the overall SVI was associated with a 0.9% increase in weekly cumulative increase in incidence rate (IRR, 1.01; 95% CI, 1.01-1.01; P < .001) and 0.5% increase in mortality rate (IRR, 1.01; 95% CI, 1.01-1.01; P < .001).
Conclusions and Relevance
In this cross-sectional study, a wide range of sociodemographic risk factors, including socioeconomic status, racial/ethnic minority status, household composition, and environmental factors, were significantly associated with COVID-19 incidence and mortality. To address inequities in the burden of the COVID-19 pandemic, these social vulnerabilities and their root causes must be addressed.
Related collections
Most cited references26
- Record: found
- Abstract: found
- Article: not found
An interactive web-based dashboard to track COVID-19 in real time
- Record: found
- Abstract: found
- Article: not found
Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis
- Record: found
- Abstract: not found
- Article: not found