- Record: found
- Abstract: found
- Article: found
Are the determinants of vertebral endplate changes and severe disc degeneration in the lumbar spine the same? A magnetic resonance imaging study in middle-aged male workers
Read this article at
Abstract
Background
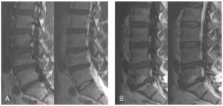
Modic changes are bone marrow lesions visible in magnetic resonance imaging (MRI), and they are assumed to be associated with symptomatic intervertebral disc disease, especially changes located at L5-S1. Only limited information exists about the determinants of Modic changes. The objective of this study was to evaluate the determinants of vertebral endplate (Modic) changes, and whether they are similar for Modic changes and severe disc degeneration focusing on L5-S1 level.
Methods
228 middle-aged male workers (159 train engineers and 69 sedentary factory workers) from northern Finland underwent sagittal T1- and T2-weighted MRI. Modic changes and disc degeneration were analyzed from the scans. The participants responded to a questionnaire including items of occupational history and lifestyle factors. Logistic regression analysis was used to evaluate the associations between selected determinants (age, lifetime exercise, weight-related factors, fat percentage, smoking, alcohol use, lifetime whole-body vibration) and Modic type I and II changes, and severe disc degeneration (= grade V on Pfirrmann's classification).
Results
The prevalences of the Modic changes and severe disc degeneration were similar in the occupational groups. Age was significantly associated with all degenerative changes. In the age-adjusted analyses, only weight-related determinants (BMI, waist circumference) were associated with type II changes. Exposure to whole-body vibration, besides age, was the only significant determinant for severe disc degeneration. In the multivariate model, BMI was associated with type II changes at L5-S1 (OR 2.75 per one SD = 3 unit increment in BMI), and vibration exposure with severe disc degeneration at L5-S1 (OR 1.08 per one SD = 11-year increment in vibration exposure).
Related collections
Most cited references26
- Record: found
- Abstract: found
- Article: not found
Disc degeneration of the lumbar spine in relation to overweight.
- Record: found
- Abstract: found
- Article: not found