- Record: found
- Abstract: found
- Article: found
Danger Zones of the Gluteal Anatomy: Improving the Safety Profile of the Gluteal Fat Grafting
Read this article at
Abstract
Introduction
Knowledge of the vascular anatomy is critical to performing safe gluteal surgery. To date, only the course of the main blood vessels within the muscles has been outlined. These findings are based on MRI and CTA images that do not conform to a topographically standardized and normalized probability distribution.
Objectives
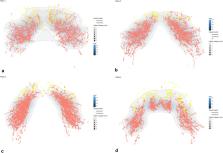
The aim of this study was to develop a three-dimensional mapping of the gluteal zones of high vascular density in relation to anatomical landmarks.
Materials and Methods
This single-center retrospective cohort analysis comprised all consecutive patients who underwent cone-beam computed tomography (CBCT) scans between January 2016 and October 2021. The location of blood vessels in the gluteal region was allometrically normalized in relation to anatomical landmarks. Moreover, the caliber and area of the blood vessels were assessed.
Results
CBCT scans of 32 patients with an average age of 64 ± 12 years (range 34–87 years) were included. Fifty-three percent were female. The median [IQR] caliber of the intramuscular gluteal vessels was 1.47 [1.15–1.88] mm, significantly greater than that of the subcutaneous vessels 1.09 [0.72–1.44] mm ( p < 0.001). Vascular density was higher intramuscularly, as 4.5% of the area of the muscle was occupied by blood vessels, as opposed to 0.3% in the adipose tissue.
Conclusion
The analysis of the CBCT scans showed a higher vascular density and larger vessels intramuscularly. We, therefore, recommend the injection of autologous fat merely to the subcutaneous plane.
Level of Evidence II
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Related collections
Most cited references44

- Record: found
- Abstract: found
- Article: found
Fat Therapeutics: The Clinical Capacity of Adipose-Derived Stem Cells and Exosomes for Human Disease and Tissue Regeneration
- Record: found
- Abstract: not found
- Article: not found
A micromechanical model for the Young’s modulus of adipose tissue

- Record: found
- Abstract: found
- Article: found