- Record: found
- Abstract: found
- Article: found
Using Self-Study and Peer-to-Peer Support to Change “Sick” Care to “Health” Care: The Patient Perspective
Read this article at
Abstract
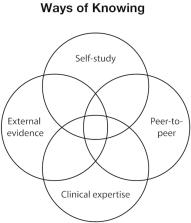
Background: Access to digital health technologies is contributing to a paradigm shift where sickcare may become authentic healthcare. Individuals can now access personal health data through wearable sensors, affordable lab screenings, genetic and genomic sequencing, and real-time health tracking apps. Personal health data access creates opportunities to study health indicators 24/7 and in real time. This is especially useful for patients with hard-to-diagnose or treat diseases, which led to a self-formed patient group called Project Apollo. Project Apollo is composed of highly motivated patients with common experiences of undiagnosed conditions, a lack of clear treatment options, and shared frustrations with navigating the U.S. healthcare system. These experiences have led the Apollo cohort to supplement their health knowledge through self-study research.
Objective: To qualify the experience and expectations of patients affiliated with Project Apollo.
Methods: A qualitative approach involved record review and semi-structured interviews. One-hour semi-structured interviews were conducted to solicit motivations, expectations, and potential barriers and facilitators to self-study followed by a brief survey on digital tool use. Interviews were digitally recorded, transcribed, and analyzed to identify themes and patterns.
Results: Participants included six females and three males ranging in age from 30 to 70+ years. Responses were organized under five key themes including: frustration with healthcare system; community support; self-study/N-of-1 research; access to experts; moving from sick to healthcare. Facilitators include motivation, albeit stemming from frustration, a safe community where patients derive support, and access to experts for guidance. Increasing awareness of clinicians about the potential value of partnering with patients who are advancing health knowledge through self-study is critical.
Conclusions: N-of-1 self-study research, coupled with community support and digital health tools, appears to be one plausible pathway to shifting the paradigm from sickcare toward patient-partnered healthcare.
Related collections
Most cited references29
- Record: found
- Abstract: not found
- Article: not found
Evidence based medicine: what it is and what it isn't

- Record: found
- Abstract: found
- Article: found
Physical, psychological and occupational consequences of job burnout: A systematic review of prospective studies
- Record: found
- Abstract: found
- Article: not found