- Record: found
- Abstract: found
- Article: not found
COVID-19-associated Evans syndrome: A case report and review of the literature
Read this article at
Abstract
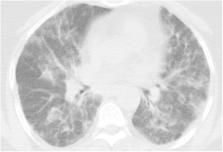
Evans syndrome is a rare condition characterized by simultaneous or sequential development of autoimmune hemolytic anemia and immune thrombocytopenia (and/or immune neutropenia). Coronavirus disease 2019 (COVID-19) may cause various hematologic conditions, such as coagulation abnormalities (e.g., bleeding or thrombosis) or cell count alterations (e.g., lymphopenia and neutrophilia). COVID-19 may also induce Evans syndrome via immune mechanisms. Here, we describe the case of a patient developing Evans syndrome shortly after COVID-19 infection. Immune thrombocytopenia and warm-type autoimmune hemolytic anemia developed simultaneously, and intravenous immunoglobulin and methylprednisolone were initially administered. Additionally, we intend to review all COVID-19-induced Evans syndrome cases currently present in the literature and emphasize the differences as well as the similarities regarding patient characteristics, relationship to COVID-19 infection, and treatment approach. Since autoimmune cytopenias are frequent in COVID-19 patients, clinicians should pay particular attention to profound and abrupt-onset cytopenias. In these circumstances, hemolysis markers such as lactate dehydrogenase, haptoglobulin, Coombs tests, etc. should be investigated, and the possibility of Evans syndrome should always be considered to ensure prompt and appropriate treatment. These factors are essential to ensure hematologic recovery and prevent complications such as thrombosis.
Related collections
Most cited references19
- Record: found
- Abstract: found
- Article: not found
Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: A meta-analysis
- Record: found
- Abstract: found
- Article: not found
