- Record: found
- Abstract: found
- Article: found
Comparative Analysis of the Safety and Functional Outcomes of Anterior versus Retropupillary Iris-Claw IOL Fixation
Read this article at
Abstract
Purpose
To compare the functional and clinical outcomes of the iris-claw intraocular lens (IOL) placed on the anterior versus posterior surface of the iris.
Patients and Methods
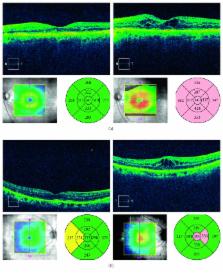
A multicenter, retrospective study. Data on eyes that underwent anterior or retropupillary iris-claw IOL implantation because of inadequate capsular support secondary to complicated cataract surgery, trauma, and dislocated/opacified IOLs since January 2015 were analyzed. For study inclusion, evaluation results had to be available in the medical records both preoperatively and at 1 and 12 months after implantation. The following parameters were compared between the groups: best-corrected distance visual acuity (BCDVA), spherical and cylindrical refractive error, endothelial cell density (ECD), central macular thickness (CMT), and percentage and type of postoperative complications.
Results
In total, 60 eyes of 60 patients aged 73 ± 13 years were included: 28 eyes (47%) involved anterior, and 32 eyes (53%) retropupillary, iris-claw IOL fixations. Preoperatively, the groups were similar in all parameters except for a significantly higher proportion of retropupillary fixations in patients who had previously experienced a closed-globe trauma ( p=0.03). The groups showed comparable improvements in BCDVA after surgery (final BCDVA: 0.34 ± 0.45 vs. 0.37 ± 0.50 logMAR in the anterior and retropupillary placement groups, respectively). During follow-up, no group difference was observed in refractive error or CMT. Both groups experienced similarly marked ECD loss and showed similar incidence of postoperative complications, with cystoid macular edema being the most common complication. Multivariable linear regression showed that BCDVA at 1 month was the best predictor of the final BCDVA.
Related collections
Most cited references18
- Record: found
- Abstract: found
- Article: not found
Simplified and safe method of sutureless intrascleral posterior chamber intraocular lens fixation: Y-fixation technique.
- Record: found
- Abstract: found
- Article: not found
Iris-claw intraocular lenses to correct aphakia in the absence of capsule support.
- Record: found
- Abstract: found
- Article: not found