- Record: found
- Abstract: found
- Article: not found
Identifying and Prioritizing Workplace Climate Predictors of Burnout Among VHA Primary Care Physicians
Read this article at
Abstract
Objective
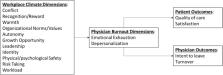
Burnout, or job-related stress, affects more than half of all US physicians, with primary care physicians (PCPs) experiencing some of the highest rates in medicine. Our study analyzes national survey data to identify and prioritize workplace climate predictors of burnout among PCPs within a large integrated health system.
Design
Observational study of annual survey data from the Veterans Health Administration (VHA) All Employee Survey (AES) for 2013–2017. AES response rate ranged from 56 to 60% during the study period. Independent and dependent variables were measured from separate random samples. In total, 8,456 individual-level responses among PCPs at 110 VHA practice sites were aggregated at the facility level by reporting year. We used the semi-automated LASSO procedure to identify workplace climate measures that were more influential in predicting burnout and assessed relative importance using the Shapely value decomposition.
Main measures
Dependent variables included two dichotomous measures of burnout: emotional exhaustion and depersonalization. Independent measures included 30 survey measures related to dimensions of workplace climate (e.g., workload, leadership, satisfaction).
Results
We identified seven influential workplace climate predictors of emotional exhaustion and nine predictors of depersonalization. With few exceptions, higher agreement/satisfaction scores for predictors were associated with a lower likelihood of burnout. The majority of explained variation in emotional exhaustion was attributable to perceptions of workload (32.6%), organization satisfaction (28.2%), and organization support (19.4%). The majority of explained variation in depersonalization was attributable to workload (25.3%), organization satisfaction (22.9%), and connection to VHA mission (20.7%).
Conclusion
Identifying the relative importance of workplace climate is important for the allocation of health organization resources to mitigate and prevent burnout within the PCP workplace. In a context of limited resources, efforts to reduce perceived workload and improve organization satisfaction may represent the biggest leverage points for health organizations to address physician burnout.
Related collections
Most cited references46
- Record: found
- Abstract: found
- Article: not found
Physician burnout: contributors, consequences and solutions
- Record: found
- Abstract: found
- Article: not found
Burnout and satisfaction with work-life balance among US physicians relative to the general US population.
- Record: found
- Abstract: not found
- Article: not found
