- Record: found
- Abstract: found
- Article: found
An implantable restorative-neurostimulator for refractory mechanical chronic low back pain: a randomized sham-controlled clinical trial
Read this article at
Abstract
Randomized, sham-controlled, double-blinded trial to demonstrate safety and efficacy of a novel, implantable restorative-neurostimulator targeting functional instability of the lumbar spine in patients with refractory mechanical chronic low back pain.
Abstract
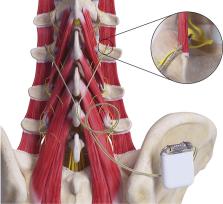
Chronic low back pain can be caused by impaired control and degeneration of the multifidus muscles and consequent functional instability of the lumbar spine. Available treatment options have limited effectiveness and prognosis is unfavorable. We conducted an international randomized, double-blind, sham-controlled trial at 26 multidisciplinary centers to determine safety and efficacy of an implantable, restorative neurostimulator designed to restore multifidus neuromuscular control and facilitate relief of symptoms ( clinicaltrials.gov identifier: NCT02577354). Two hundred four eligible participants with refractory mechanical (musculoskeletal) chronic LBP and a positive prone instability test indicating impaired multifidus control were implanted and randomized to therapeutic (N = 102) or low-level sham (N = 102) stimulation of the medial branch of the dorsal ramus nerve (multifidus nerve supply) for 30 minutes twice daily. The primary endpoint was the comparison of responder proportions (≥30% relief on the LBP visual analogue scale without analgesics increase) at 120 days. After the primary endpoint assessment, participants in the sham-control group switched to therapeutic stimulation and the combined cohort was assessed through 1 year for long-term outcomes and adverse events. The primary endpoint was inconclusive in terms of treatment superiority (57.1% vs 46.6%; difference: 10.4%; 95% confidence interval, −3.3% to 24.1%, P = 0.138). Prespecified secondary outcomes and analyses were consistent with a modest but clinically meaningful treatment benefit at 120 days. Improvements from baseline, which continued to accrue in all outcome measures after conclusion of the double-blind phase, were clinically important at 1 year. The incidence of serious procedure- or device-related adverse events (3.9%) compared favorably with other neuromodulation therapies for chronic pain.
Related collections
Most cited references85
- Record: found
- Abstract: found
- Article: not found
Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L)
- Record: found
- Abstract: found
- Article: not found
What low back pain is and why we need to pay attention
- Record: found
- Abstract: not found
- Article: not found