- Record: found
- Abstract: found
- Article: found
Editorial: Fascia as a multi-purpose structure of connective tissue - dysfunction, diagnostics and treatment
editorial
14 August 2024
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
For many years, the fasciae have been considered only as a “white envelope for the
muscles”, and very little attention has been given to their macroscopic and histological
anatomy. With the last researches it is clear that we can recognized many fasciae,
each one with specific features: the superficial fascia, the muscular fasciae, the
visceral fasciae and the neural fasciae. The superficial fascia is rich in elastic
fibers (1), it is adaptable and strongly connected with the skin (2), it envelops
and protect the superficial vessels and nerves and probably plays a key role in lymphatic
drainage (3), and in tissue healing and regeneration processes (4). The muscular (or
deep) fasciae are distinguished in two big groups: the aponeurotic fasciae, that work
as a bridge connecting different muscles, and the epimysial fasciae, specific for
each muscle. The deep fasciae are formed by collagen fibers organized in layers, and
each layer is separated by the closer one by loose connective tissue, rich in water
and hyaluronan (HA) (5). The collagen fibers define the mechanical behavior of fasciae,
the hyaluronan defines the tissue hydration and the ability of glide. All these elements
could be altered by trauma, bad posture, immobilization. The visceral fasciae envelope
the viscera and define their mobility and motility (6). They have a rich autonomic
innervation and connect the organs to the locomotor system in very precise points.
Finally, also the meningeal layers could be considered specialized fasciae.
The fasciae are very well-innerved (more than muscles, tendons, and joints), both
with sensitive an autonomic innervation, so much to be considered a sensory organ
(7). We can distinguished three different type of innervation inside fasciae:
Free nerve ending forming a network, totally embedded in the fasciae, and able to
perceive every change in the fascial tension. These receptors have a key role in proprioception
and in the perception of the motor directions, but also they could be able to perceive
pain (8).
Autonomic fibers, they are around 35% in the superficial fascia, a little less in
the deep fasciae, much more in the visceral ones. They are present above all around
the main vessels, and consequently they are responsible of the regulation of the blood
flow inside the fasciae, but also in the middle of the connective tissue, and consequently
they could be involved in the fibrotic process of fascial tissue (9).
The muscle spindles. They are a specific innervation of the epimysial fasciae. Indeed
these corpuscles are totally embedded in the perimysium, and their capsule is nothing
more than a doubling of the perimysium around the intrafusal fibers. Muscle spindles
inform the Central Nervous System (CNS) of the continually changing status of muscle
tone, movement, loss of normal elasticity, position of body parts, absolute length
of muscle and rate of change (velocity) of the length of the muscle. In order for
a muscle spindle to function it must be able to lengthen, shorten and glide to allow
its annulospiral and flower spray organs to be stretched to report accurate information
to the CNS (10), and this is made possible by the epimysial fascia.
So, fasciae could be considered a key element in peripheral motor coordination and
proprioception, but also of interoception. At the same time, altered (restricted,
densified) fasciae are responsible for chronic stiffness, decreased strength and abnormal
movement patterns (loss of motor direction of bodily segments), bad motility of the
internal organs, altered lymphatic drainage (11).
Besides, the fasciae could be subjected to different types of alterations, some are
clearly visible with standard imaging evaluations, other need a biopsy to be understood.
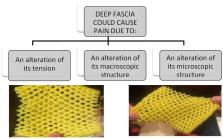
In a schematic way, we can distinguish three different conditions (Figure 1):
The fascia has only an anomalous tension, due to the overstretching due to the underlying
muscles that insert into it or to postural alteration. In this case the fascia is
healthy, but the nerve receptors inside are constantly triggered. Wilke et al. (12)
demonstrated the strain transfer along fasciae. In particular, the Authors checked
the range of motion of the neck in 26 healthy participants before and after the stretching
of the inferior limbs. After stretching, the cervical Range of Motion (ROM) was improved,
demonstrating the anatomical continuity of the fasciae of inferior limbs and neck.
From a clinical point of view, it means that a trauma or a tension in the inferior
limbs can affect the neck mobility, and consequently some patients maybe don't answer
to our treatments because they are addressed at the wrong area. Further, it means
that it is important to assess in a global way a patient with myofascial pain, because
the fascial alteration could be far away from the site of pain.
The fascia has macroscopic alterations, such as a scar after surgery or trauma. These
alterations could be seen with the standard ultrasound evaluation, but also with Magnetic
Resonance Imaging (MRI) and TC. Stecco et al. (13) evaluated 25 subjects with chronic
ankle instability with MRI, demonstrating in 21 patients specific alterations of the
ankle retinacula (that are fascial thickenings), such as edema, interruption of continuity,
thickening or adhesion to the subcutaneous layers. These alterations were observed
separately or in association. In a recent review, Pirri et al. (14) listed all the
Ultrasound (US) parameters that can be altered in the fasciae and that can allow to
do a diagnosis of fascial pathology: thickness, echogenicity, stiffness, deformation,
shear strain, and displacement.
The fascia can be altered in their molecular components, such as the amount of collagen
and elastic fibers, or of hyaluronan, or in the density of innervation and vascularization.
In this case, the imaging evaluations show a standard macroscopic organization of
the fasciae, and only the biopsy can highlight the alteration. In the last years Fede
et al. (15) demonstrated as the quantity of elastic and collagen fibers vary with
aging, as happens in all the subcutaneous tissues. It was recently demonstrated that
different levels of estrogenic hormones can modulate the production of collagen I,
collagen III and fibrillin (16). It seems that post-menopausal fasciae have more collagen
type I (8.4 vs. 5.2% in control) and less collagen III (1.5 vs. 2.4%), explaining
why the fasciae become more rigid with aging. On the contrary, fasciae become more
elastic during pregnancy, with increased amounts of collagen-III (6.7%) and fibrillin
(3.6%, compared to 0.5% of the control) and a corresponding decrease of collagen I
(1.9%). Mechanical inputs, such as extracorporeal shock wave, also seems to change
the fiber composition in fasciae, activating gene expression for transforming growth
factor β1 and collagen types I and III (17, 18). With diabetes there are chronic alterations
of the connective tissue, with a thickening of the collagen fibers and a fragmentation
of the elastic fibers, leading to fascial stiffness (19, 20). The synthesis of the
collagen type III fibers increases in diabetic subjects, whereas the synthesis of
collagen type I fibers decreases. Furthermore, Extracellular Matrix (ECM) turnover
in diabetes patients is affected by chronic hyperglycemia, determining the accumulation
of larger quantities of collagen, resulting in ECM thickening. Fantoni et al. observed
(21) a relationship between fascial pathology and hip osteoarthritis (OA): in OA patients
Authors demonstrated an increase in Collagen I (COL I), along with the reduction of
Collagen III (COL III) and HA, leading to fascial stiffening, which could alter fascial
mechanics and be linked to the development and symptoms of OA.
Figure 1
Fascia could cause pain in different modalities, and they required different types
of treatment and different way to make diagnosis. One of the most common cause of
fascial pain is an alteration of the fascial tension, that cause a deformation of
the fascial free nerve ending.
Another element that can alter the microanatomy of fasciae are the myofibroblasts.
According to Schleip et al. (22), myofibroblasts are present in all fasciae, but cell
density increases in many pathological conditions, such as palmar fibromatosis, Morbus
Ledderhose, hypertrophic scars, and similar fascial fibrotic conditions, but also
in chronic low back pain, where myofibroblasts are associated with an augmented occurrence
of (micro-) injuries and related cellular repair processes. It seems that fascial
alteration could be a trigger for the transformation of fibroblasts into myofibroblasts
but, due to their contractile activity, myofibroblasts further increase fascial tension
creating a loop that progressively aggravates the problem. Fasciae express also cannabinoid
receptors [both Cannabinoid 1 and 2 (CB1 and CB2)] and their stimulation seems to
induces the production of hyaluronan-rich vesicles, leading to greater tissue fluidity
(23, 24).
To conclude, we think that it is time that fasciae will be considered in the clinical
setting because there are many evidences that they can be a source of pain. The various
aspects of diagnosing fascia disorders and the effectiveness of the applied therapy
methods have been confirmed in studies published in this Research Topic, for the treatment
of allergies (Liu et al.), joint pain and joint disorders (Liu and Wang; Rogers et
al.) and the most common back pain (Brandl et al.), highlighting that the fascia should
be considered for diagnosis and treatment in heterogeneous and diverse clinical pictures.
However, it is important to consider that, to understand the fascial alteration and
how improve a fascial alteration, it is important to consider that fasciae form a
three dimensional network and consequently the point at which the patient feels pain
often does not correspond at the origin of the fascial problem. This implies that
if we evaluate with ultrasound, MRI or other instruments the fascia where the patient
feels pain, probably we are not able to see any alteration, but this does not automatically
mean that this is not a fascial problem. Besides, the assessment of a patient with
fascial problems required always a global analysis, considering previous trauma and
previous unbalance conditions of the fasciae.
Related collections
Most cited references24
- Record: found
- Abstract: found
- Article: not found
Biological effects of extracorporeal shock waves on fibroblasts. A review.
Roberto Frairia, Laura Berta (2011)
- Record: found
- Abstract: found
- Article: not found
Fascial Disorders: Implications for Treatment.
Antonio Stecco, Robert Stern, Ilaria Fantoni … (2016)
- Record: found
- Abstract: not found
- Article: not found
Remote effects of lower limb stretching: preliminary evidence for myofascial connectivity?
Jan Wilke, Winfried Banzer, Lutz Vogt … (2016)