- Record: found
- Abstract: found
- Article: found
Evaluating the effect of injecting triamcinolone acetonide in two sessions for preventing esophageal stricture after endoscopic submucosal dissection
Read this article at
Abstract
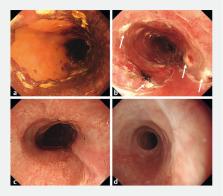
Background and study aims Several previous reports indicate that endoscopic injection of triamcinolone acetonide (TA) after widespread endoscopic submucosal dissection (ESD) is effective for preventing esophageal stricture. We investigated the efficacy of injecting TA in two sessions for preventing stricture formation post-ESD.
Patients and methods Sixty-six consecutive patients with widespread mucosal defects that affected more than three-fourths of the circumference of the esophagus were included. The study group (n = 40) received TA injections over two sessions: immediately after and 14 days after ESD. The control group (n = 26) did not receive a TA injection. This study was performed retrospectively against historical controls. The primary endpoint of this study was frequency of stricture after TA injection. The secondary endpoint was number of required endoscopic balloon dilations (EBDs) after TA injection.
Results The post-ESD stricture rate among patients who had subcircumferential mucosal defects was 45.7 % in the study group (16/35 patients), which was significantly lower than the rate of 73.9 % in the control group (17/23 patients; P = 0.031). The number of EBD procedures required was significantly lower in the study group (median 0, range 0 – 7) than in the control group (median 4, range 0 – 20; P < 0.001). There was no significant difference between the study and control groups among the patients who had full circumferential mucosal defects.
Conclusion This study showed that performing two sessions of TA injection is an effective and safe treatment for prevention of esophageal stricture following subcircumferential ESD.
Related collections
Most cited references21
- Record: found
- Abstract: found
- Article: not found
Predictors of postoperative stricture after esophageal endoscopic submucosal dissection for superficial squamous cell neoplasms.
- Record: found
- Abstract: found
- Article: not found
Endoscopic submucosal dissection of early esophageal cancer.
- Record: found
- Abstract: found
- Article: not found