- Record: found
- Abstract: found
- Article: found
Magnitudes and Correlates of Human Immunodeficiency Virus, Hepatitis B Virus, and Syphilis among Pregnant Mothers Attending Antenatal Care in Addis Ababa, Ethiopia
Read this article at
Abstract
Background
Human immunodeficiency virus (HIV), hepatitis B virus (HBV), and syphilis are major sexually transmitted infections (STIs) among the general population in Ethiopia, which in turn result in a wide range of adverse pregnancy outcomes. Hence, it is important to determine the seroprevalence and risk factors of HIV, HBV, and syphilis infection among pregnant mothers attending antenatal care in Addis Ababa, Ethiopia.
Method
A cross-sectional study was conducted among 286 pregnant women from February 1, 2021, to March 30, 2021, in four selected public hospitals in Addis Ababa. Sociodemographic, risky sociocultural, behavioral, and hospital-related factors were collected using an interview-administered questionnaire. Detection of anti-HIV antibodies, hepatitis B surface antigen (HBsAg), and rapid plasma reagin (RPR) for syphilis was conducted. A binary logistic regression analysis was used to determine predictors of STIs using SPSS version 25.
Result
A total of 281 pregnant mothers with a mean age of 27.5 (SD 4.6) completed the study. Among the participants, the seroprevalence rates of HIV, HBV, and syphilis were 15 (5.3%), 9 (3.2%), and 5 (1.8%), respectively. Twenty six (9.3%) of the participants tested positive for any one of the STIs, and 3 (1.1%) of the women had HIV and syphilis coinfections. History of multiple sexual partners (AOR 3.42, 95% CI: 1.6-11.63) and STIs (AOR 3.7; 95% CI: 1.70-13.45) were significantly associated with HIV infection. Likewise, history of abortion (AOR 7.65, 95% CI: 1.17-49.74), tattooing (AOR 9.72, 95% CI: 1.41-66.73), and rape (AOR 9.72, 95% CI: 1.41-66.73) were significantly associated with hepatitis B virus infection. Husband history of multiple sexual partners (AOR 20.9, 95% CI: 1.8-241.8) was significantly associated with syphilis infection. The educational level of participants, history of tattooing (AOR 6.24, 95% CI: 1.79-21.7), and history of multiple sexual partners (AOR 5.15, 95% CI: 1.68-15.7) were independent predictors of infection with any one of the STIs.
Related collections
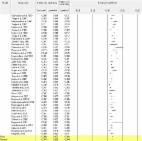
Most cited references46

- Record: found
- Abstract: found
- Article: found
Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016

- Record: found
- Abstract: found
- Article: found
Global, regional, and national incidence, prevalence, and mortality of HIV, 1980–2017, and forecasts to 2030, for 195 countries and territories: a systematic analysis for the Global Burden of Diseases, Injuries, and Risk Factors Study 2017
- Record: found
- Abstract: found
- Article: found