- Record: found
- Abstract: found
- Article: not found
If not now, when? COVID-19, lived experience, and a moment for real change
discussion
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
In a Position Paper published in The Lancet Psychiatry, Carmen Moreno and colleagues
1
recommended bolder language and framing with respect to the meaningful involvement
of service users in mental health planning, policy, and research in the wake of COVID-19.
It is always gratifying to hear enthusiasm for goals the user and survivor research
movement has long fought for. We were similarly gratified to read an Editorial in
The Lancet Psychiatry arguing for pressure from service users to more actively shift
societal discourse.
2
And yet, as welcome as these statements are, we worry that the primary problem we
are all up against is not a paucity of articulated support for service-user involvement
but rather the gap between rhetoric and reality.
Our collective experience suggests that both before, and now many months into, the
COVID-19 pandemic, meaningful service-user involvement remains unevenly implemented
in some places, and non-existent in others. In some regions, involvement could be
reduced from pre-COVID-19 levels, whereas in others, attestations to the importance
of inclusion might have long been unaccompanied by concrete action. The same sentiment—anger
and frustration about decades of inaction—has also been at the forefront of the Extinction
Rebellion, March for our Lives, and Black Lives Matter movements. At a specific point,
one feels the need to say “enough talk”. And if there was ever a moment when we, as
a field, might take deeper stock of where we really want to head, it is arguably now.
Involvement efforts are too often accompanied by empty promises, insufficient funding
or commitment, and superficial gestures (eg, membership on advisory boards), with
no real power to set agendas, influence decision making, or bring about structural
change.3, 4, 5
Concretely then, what actions might be taken at this pivotal cultural moment? As activists
across multiple under-represented social groups have long argued, leadership roles
and power over decision making are fundamental.4, 5 From a systems perspective, this
situation means addressing barriers specific to both academic training and advancement
and research funding. Beginning with addressing barriers in academia, explicit proactive
support for students and investigators with lived experience must be provided across
the training pipeline, from undergraduate studies through to independence as mid-career
investigators. Ideally, such support would be pursued with the primary goal of supporting
junior scholars to ultimately obtain their own grants as primary investigators, particularly
in fields in which extramural funding is sine qua non for promotion and advancement.6,
7 In supporting such trajectories, senior researchers must take care to ensure that
service-user trainees and researchers, when included in studies and grants, are not
there primarily to check a box or shore-up involvement plans, but to substantively
shape research activities and, above all, advance their own careers and research agendas.
Attention to diversity within this pipeline is also important, certainly of race,
ethnicity, gender, sexual orientation, and class, but also with respect to level of
disability and intersectional experiences of homelessness, incarceration, discrimination,
addiction, and poverty.
8
Research funders, in turn, must implement safeguards against discrimination, communicate
and enforce robust expectations for service-user involvement and leadership in research
proposals, and ensure that established bodies of research do not become barriers to
authentic community-led innovation.4, 9 Too often, funding processes re-inscribe existing
hierarchies and established interventions by rewarding proposals that build on, and
hew to, existing published work. High-risk high-reward funding streams are typically
present in the basic and translational sciences or new research areas such as digital
health, with such language rarely used to refer to or fund user-led innovations. To
achieve deeper change, funders must be open to new ideas and new directions, guided
by those on the receiving end of services.
Is the above pipeline merely a pipe dream? Our belief is that senior researchers,
large research centres, and training programmes could readily take the steps described
above, including substantially greater hiring, mentoring, and support of under-represented
students and researchers with lived experience. Were it a priority, research funding
bodies could—with relatively minor modifications to programme announcements—directly
support meaningful involvement and leadership.
Failure to do the above is neither a fault of structures over which the field has
no control nor stigma among some other group, but it is an individual choice on the
part of those in positions of power to remain stagnant and perpetuate processes and
lines of research that marginalise the experiences and knowledge of the very populations
this research aims to serve. Rather than bold language, we call for bold action.
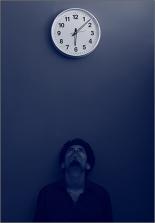
© 2020 Wilsan U:Unsplash
2020
Since January 2020 Elsevier has created a COVID-19 resource centre with free information
in English and Mandarin on the novel coronavirus COVID-19. The COVID-19 resource centre
is hosted on Elsevier Connect, the company's public news and information website.
Elsevier hereby grants permission to make all its COVID-19-related research that is
available on the COVID-19 resource centre - including this research content - immediately
available in PubMed Central and other publicly funded repositories, such as the WHO
COVID database with rights for unrestricted research re-use and analyses in any form
or by any means with acknowledgement of the original source. These permissions are
granted for free by Elsevier for as long as the COVID-19 resource centre remains active.
Related collections
Most cited references8
- Record: found
- Abstract: found
- Article: found
How mental health care should change as a consequence of the COVID-19 pandemic
Carmen Moreno, Til Wykes, Silvana Galderisi … (2020)
- Record: found
- Abstract: found
- Article: found
Six ‘biases’ against patients and carers in evidence-based medicine
Trisha Greenhalgh, Rosamund Snow, Sara Ryan … (2015)
- Record: found
- Abstract: found
- Article: not found
Close to the bench as well as at the bedside: involving service users in all phases of translational research.
Felicity Callard, Diana Rose, Til Wykes (2012)
