- Record: found
- Abstract: found
- Article: found
Angiopoietin-like 8 (ANGPTL8) as a potential predictor of NAFLD in paediatric patients with Prader-Willi Syndrome
Read this article at
Abstract
Purpose
Angiopoietin-like 8 (ANGPTL8) is a liver- and adipose tissue-produced protein that predicts non-alcoholic fatty liver disease (NAFLD) and altered metabolic homeostasis in the general population as well as in persons with common and genetic obesity, including the Prader–Willi syndrome (PWS). However, its metabolic correlate in paediatric patients with respect to PWS is unknown.
Methods
This cross-sectional study investigated circulating ANGPTL8 and adipocytokines levels in 28 PWS and 28 age-, sex- and BMI-matched children and adolescents (age, 7.0–17.8y) in relation to NAFLD and metabolic homeostasis assessed by OGTT, paediatric metabolic index (PMI) and fatty liver index (FLI), liver ultrasonography (US), as well as dual-energy X-ray absorptiometry (DEXA) for analysis of fat (FM) and fat-free mass (FFM).
Results
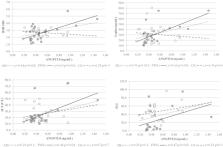
At the set level of significance, PWS children showed lower values of FFM ( p < 0.01) but healthier insulin profiles ( p < 0.01) and PMI values ( p < 0.05) than matched controls. By US, the prevalence of NAFLD was similar between groups but less severe in PWS than controls. Analysis of ANGPTL8 levels showed no difference between groups, yet only in PWS ANGPTL8 levels were associated with ALT levels, FLI values and NAFLD. In stepwise multivariable regression analysis on merged data, ANGPTL8 levels were independently predicted by BMI SDS, leptin levels and NAFLD.
Related collections
Most cited references51
- Record: found
- Abstract: not found
- Article: not found
The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases.
- Record: found
- Abstract: found
- Article: not found
Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man.

- Record: found
- Abstract: found
- Article: found