- Record: found
- Abstract: found
- Article: found
RISK ASSESSMENT IN PREGNANCY AMONG WOMEN AGED OVER FORTY
Read this article at
SUMMARY
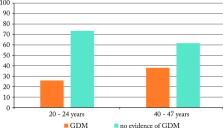
The objective of this study was to assess the relationship between women’s age and risk of pregnancy-related complications. The study was a retrospective cohort analysis of the pregnancy-related complications and outcomes between two age groups of parturient women. Categorical data were expressed as absolute and relative frequencies. Statistical analysis was performed using χ 2-test. The incidence of gestational diabetes was higher in the 40-47 age group as compared with the 20-24 age group. The rates of hypertension, preeclampsia, intrahepatic cholestasis of pregnancy and hypothyroidism did not differ between the two groups. The rates of labor induction, oxytocin use, vaginal delivery, and need for episiotomy were higher in younger age group. Dystocia and breech presentation as indications for cesarean section were more common among younger women. According to study results, the risk of gestational diabetes and rates of cesarean delivery increased with advanced maternal age.
Related collections
Most cited references34
- Record: found
- Abstract: found
- Article: not found
Hyperglycemia and adverse pregnancy outcomes.

- Record: found
- Abstract: found
- Article: found
Advanced maternal age and adverse pregnancy outcomes: A systematic review and meta-analysis
- Record: found
- Abstract: found
- Article: not found