- Record: found
- Abstract: found
- Article: found
Definitive 3D-CRT for clinically localized prostate cancer: modifications of the clinical target volume following a prostate MRI and the clinical benefits
Read this article at
Abstract
Purpose
To evaluate the modifications of the tumor stage and clinical target volume following a prostate magnetic resonance imaging (MRI) to evaluate the tumor (T) staging, and the clinical benefits for prostate cancer.
Methods
A total of 410 patients with newly diagnosed and clinically localized prostate cancer were retrospectively analyzed. The patients were treated with definitive three-dimensional conformal radiotherapy (3D-CRT). In all of the patients, digital rectal examination, transrectal ultrasound, prostate biopsy and computed tomography were performed to evaluate the clinical stage. Of the 410 patients, 189 patients had undergone a prostate MRI study to evaluate the T staging, and 221 patients had not.
Results
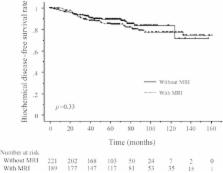
Modification of the T stage after the prostate MRI was seen in 39 (25%) of the 157 evaluable patients, and a modification of the risk group was made in 14 (9%) patients. Eventually, a modification of the CTV in 3D-CRT planning was made in 13 (8%) patients, and 10 of these had extracapsular disease. Most of the other modifications of the T staging were associated with intracapsular lesions of prostate cancer which did not change the CTV. There were no significant differences in the biological relapse-free survival between the patients with and without a prostate MRI study.
Conclusions
Modification of the CTV were recognized in only 8% of the patients, most of whom had extracapsular disease, although that of the T stage was seen in approximately one-quarter of the patients. Prostate MRI should only be selected for patients with a high probability of extracapsular involvement.
Related collections
Most cited references28
- Record: found
- Abstract: found
- Article: not found
Advances in magnetic resonance imaging: how they are changing the management of prostate cancer.
- Record: found
- Abstract: found
- Article: not found