- Record: found
- Abstract: found
- Article: not found
BMI Cut Points to Identify At-Risk Asian Americans for Type 2 Diabetes Screening
review-article
William C. Hsu
1
,
,
Maria Rosario G. Araneta
2 ,
Alka M. Kanaya
3 ,
Jane L. Chiang
4 ,
Wilfred Fujimoto
5
13 December 2014
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
Asian American Population
According to the U.S. Census Bureau, an Asian is a person with origins from the Far
East (China, Japan, Korea, and Mongolia), Southeast Asia (Cambodia, Malaysia, the
Philippine Islands, Thailand, Vietnam, Indonesia, Singapore, Laos, etc.), or the Indian
subcontinent (India, Pakistan, Bangladesh, Bhutan, Sri Lanka, and Nepal); each region
has several ethnicities, each with a unique culture, language, and history. In 2011,
18.2 million U.S. residents self-identified as Asian American, with more than two-thirds
foreign-born (1). In 2012, Asian Americans were the nation’s fastest-growing racial
or ethnic group, with a growth rate over four times that of the total U.S. population.
International migration has contributed >60% of the growth rate in this population
(1). Among Asian Americans, the Chinese population was the largest (4.0 million),
followed by Filipinos (3.4 million), Asian Indians (3.2 million), Vietnamese (1.9
million), Koreans (1.7 million), and Japanese (1.3 million). Nearly three-fourths
of all Asian Americans live in 10 states—California, New York, Texas, New Jersey,
Hawaii, Illinois, Washington, Florida, Virginia, and Pennsylvania (1). By 2060, the
Asian American population is projected to more than double to 34.4 million, with its
share of the U.S. population climbing from 5.1 to 8.2% in the same period (2).
Overweight/Obesity and Type 2 Diabetes Risk for Asian Americans
Although it is clear that increased body weight is a risk factor for type 2 diabetes,
the relationship between body weight and type 2 diabetes is more properly attributable
to the quantity and distribution of body fat (3–5). Abdominal circumference and waist
and hip measurements, although highly correlated with cardiometabolic risk (6,7),
do not differentiate subcutaneous from visceral adipose abdominal depots and are subject
to interobserver variability. Imaging and other approaches can be used to more accurately
assess fat distribution and quantify adiposity (4,8), but they are not readily available,
economical, or useable on a large scale. Therefore, the measurement of body weight
with various corrections for height is frequently used to assess risk for obesity-related
diseases because it is the most economical and practical approach in both clinical
and epidemiologic settings (9). The most commonly used measure is Quetelet’s index
or BMI, defined as weight ÷ height2, with weight in kilograms and height in meters.
However, BMI does not take into account the relative proportions of fat and lean tissue
and cannot distinguish the location of fat distribution (10,11).
The clinical value of measuring BMI from a diabetes diagnosis perspective lies in
whether this measure can identify individuals who may have undiagnosed diabetes or
may be at increased future risk for diabetes. In addition, measuring BMI also is important
for managing diabetes for the purpose of weight control. BMI cutoffs have been established
to identify overweight (BMI ≥25 kg/m2) or obese (BMI ≥30 kg/m2) individuals (12).
However, these are based on information derived from the general population, based
on risk of mortality, without consideration for racial or ethnic specificity and were
not determined to specifically identify those at risk for diabetes. Recently, the
U.S. Centers for Disease Control and Prevention presented initial findings from an
oversampling of Asian Americans in the 2011–2012 National Health and Nutrition Examination
Survey. These data, utilizing general population criteria for obesity, showed the
prevalence of obesity in Asian Americans was only 10.8% compared with 34.9% in all
U.S. adults (13). Paradoxically, many studies from Asia, as well as research conducted
in several Asian American populations, have shown that diabetes risk has increased
remarkably in populations of Asian origin, although in general these populations have
a mean BMI significantly lower than defined at-risk BMI levels (14,15). Moreover,
U.S. clinicians who care for Asian patients have noticed that many with diabetes do
not meet the published criteria for obesity or even overweight (16).
Epidemiologic studies have shown that there is a relationship between BMI and diabetes
risk in Asians, but this risk is shifted to lower BMI values (17). At similar BMI
levels, diabetes prevalence has been identified as higher in Asians compared with
whites (18). This paradox may be partly explained by a difference in body fat distribution:
there is a propensity for Asians to develop visceral versus peripheral adiposity,
which is more closely associated with insulin resistance and type 2 diabetes than
overall adiposity (19). Additionally, Asians of both sexes have been shown to have
a higher percentage of body fat at any given BMI level compared with non-Hispanic
whites; this suggests differences in body composition that may contribute to variations
in diabetes prevalence (10).
Defining the Issue
The established definitions of at-risk BMI for overweight and obesity appear to be
inappropriate for defining diabetes risk in Asian Americans. Thus, there is a need
to examine the existing literature to determine what might constitute at-risk BMI
levels for Asian Americans. The clinical relevance is to clarify the use of BMI as
a simple initial screening tool to identify Asian Americans who may have diabetes
(diagnosis) or be at risk for future diabetes (to implement prevention measures).
Also of importance is the use of specific BMI cut points to identify Asian Americans
who are eligible for weight-reduction services or treatment reimbursable by payers.
Available data from Asia support the notion that Asians are already at risk for many
obesity-related disorders even if they do not reach the BMI values associated with
overweight or obesity in non-Asian populations (14). Population-wide weight gain is
occurring throughout Asia. This has been attributed to environmental influences such
as dietary changes and reductions in physical activity commonly associated with living
in a Western culture (17). However, the impact of actually living in a Western culture
may be different or more adverse than the effect of living in the native homeland
and experiencing some of the lifestyle features representative of a Western culture.
Rather than relying on hypothetical influences surmised from data from Asia, it is
better therefore to directly examine the relationship of BMI to metabolic disorders
such as type 2 diabetes among Asians living in the U.S. Although the U.S. Census has
historically combined Asians, Native Hawaiians, and other Pacific Islanders, there
are significant differences in physiology and body composition between Asians and
the other two groups, so this review will focus only on examining studies in Asian
Americans.
Asian American Studies of Type 2 Diabetes and Overweight/Obesity
Prospective cohort or longitudinal studies are the most suitable designs to measure
type 2 diabetes incidence and delineate the relationship between BMI and diabetes.
This research requires clinical ascertainment of BMI and nondiabetic status at baseline,
followed by periodic reascertainment for a defined follow-up period or until diabetes
is diagnosed. Glucose tolerance status should be evaluated by blood test, preferably
including a 2-h 75-g oral glucose tolerance test (OGTT). This recommendation is based
on numerous studies, including research on Asian Americans, indicating that OGTT detects
a greater number of individuals with diabetes compared with fasting glucose criteria
(20–22). This type of longitudinal study design enables 1) identification of baseline
BMI values associated with increased diabetes risk over a defined follow-up and 2)
capture of BMI data at the earliest time point following diabetes diagnosis. The sensitivity
and specificity of BMI cut points can then be identified using analytic techniques
such as receiver operating characteristic curves or rate of misclassification.
Historically, such prospective cohort data are uncommon in Asian American populations.
The majority of peer-reviewed publications on diabetes among Asian Americans are cross-sectional
studies in which BMI, calculated from self-reported weight and height, and diabetes
status are assessed simultaneously. In 2004, data from the Behavioral Risk Factor
Surveillance System (BRFSS) showed that the odds of prevalent diabetes were 60% higher
for Asian Americans than non-Hispanic whites after adjusting for BMI, age, and sex
(23). The National Health Interview Survey (NHIS; 1997–2008 data) (24) found that
the odds of prevalent diabetes were 40% higher in Asian Americans relative to non-Hispanic
whites after adjusting for differences in age and sex. In fully adjusted logistic
regression models including an adjustment for BMI as a categorical variable (underweight/normal
weight: BMI <23 kg/m2, overweight: 23 ≤ BMI < 27.5 kg/m2, and obese: BMI ≥27.5 kg/m2),
Asian Americans remained 30–50% more likely to have diabetes than their non-Hispanic
white counterparts (24). Additionally, regional studies, such as the New York City
Health and Nutrition Examination Survey (25), have confirmed that Asian residents
in New York City had the highest levels of dysglycemia (diabetes and prediabetes combined)
of any race/ethnicity based on prior history or fasting glucose measurement. By disaggregating
subgroups from these studies, investigators found that South Asians consistently had
the highest diabetes prevalence compared with other Asian subgroups and non-Hispanic
whites (26). Although informative, these studies’ cross-sectional designs were unable
to identify BMI at the time of diabetes diagnosis thereby indicating minimum BMI cut
points when diabetes is newly diagnosed.
A systematic review by Staimez et al. (27) summarized findings from 97 publications
(1988–2009) on the prevalence of overweight, obesity, and diabetes among specific
Asian American subgroups, including Chinese, Filipinos, Koreans, South Asians, and
Vietnamese. Almost all the articles reviewed for this publication reported cross-sectional
data for the variables of interest, and only two provided longitudinal data that were
incorporated in the conclusion. These earlier studies reported tremendous heterogeneity
in diabetes prevalence, ranging from 3.9 to 32.9% in Asian Indians, 1.0–11.3% among
South Asians, 2.2–28.0% in Chinese, 3.7–30.9% among Filipinos, 5.3–15.6% in Vietnamese,
and 10.0–18.1% among Koreans (27). Similar heterogeneity was reported for obesity
prevalence. As the objectives, age and sex distribution, recruitment methods, and
ascertainment of BMI and diabetes varied broadly among these studies, it is not feasible
to use these data to identify BMI cut points for diabetes manifestation. To do this,
it is imperative to establish BMI levels that place populations at risk for diabetes
prior to diabetes diagnosis as weight loss may occur either with undiagnosed diabetes
or following diagnosis due to glycosuria or treatment with lifestyle intervention
or pharmacologic agents that promote weight loss.
Since publication of the article by Staimez et al. (27), prospective cohort studies
on diabetes incidence among Asians in North America (comprising the U.S. and Canada)
have been limited to just five prospective cohorts (based on a PubMed search of the
English literature published since 2009). Table 1 summarizes the prospective studies
that have reported incident diabetes rates in Asian American populations. We reviewed
these studies, based on whether data were analyzed by specific Asian ethnicity (disaggregated)
or not (aggregated).
Table 1
Prospective cohort studies (2009–2013) reporting incident diabetes in Asian American
populations
Reference
Study, location, and follow-up
Sample size
Mean age, years
BMI, kg/m2
Diabetes ascertainment method
Diabetes incidence
Aggregated data
Ma et al., 2012 (28)
Women’s Health Initiative (1993–2009)
Asian*: 4,190
Asian: 63.0 (7.5)
Asian: 24.8 (4.6)
Self-report: physician prescribed “pills or insulin shots for diabetes”
Cumulative incidence %
Black: 14,618
Black: 61.6 (7.1)
Black: 31.2 (6.7)
Asian: 10.6
Hispanic: 6,484
Hispanic: 60.2 (6.8)
Hispanic: 29.1 (5.8)
Black: 17.0
40 centers throughout the U.S.
White: 133,541
White: 63.6 (7.2)
White: 27.6 (5.8)
Hispanic: 14.6
Follow-up: 10.4 years
Incidence rate (per 1,000 person-years)
Asian: 1.13
Black: 1.87
Hispanic: 1.67
White: 0.82
Disaggregated data
Karter et al., 2013 (29)
DISTANCE studyNorthern California Mean follow-up: 1 year
1,704,363 Kaiser Permanente Northern California members with known ethnicity
Filipino: 49.1 (16.2)
Mean BMI at baseline
Based on medical records: ICD-9: 250 (inpatient or two or more outpatient diagnoses)Either
FPG ≥126 mg/dL; random or postchallenge glucose ≥200 mg/dLPrescription for insulin
or oral antihyperglycemic medications
Age- and sex-adjusted prevalence %
Filipino: 82,781
Chinese: 51.6 (16.8)
Filipino: 26.6 (4.7)
Filipino: 16.1
Chinese: 68,831
Japanese: 58.7 (17.7)
South Asian: 26.4 (4.7)
South Asian: 15.9
Japanese: 16,032
South Asian: 43.4 (15.0)
SE Asian: 26.4 (5.2)
SE Asian: 10.5 Japanese: 10.3 Korean: 9.9 Vietnamese: 9.9 Chinese: 8.2 White: 7.3
South Asian: 6,768
SE Asian: 37.7 (12.2)
Japanese: 25.4 (4.9)
SE Asian: 1,876
Korean: 49.6 (15.7)
Korean: 24.9 (4.2)
Korean: 1,130
Vietnamese: 39.5 (11.6)
Vietnamese: 23.9 (4.1)
Vietnamese: 1,671
White: 53.6 (18.0)
Chinese: 24.2 (4.0)
White: 968,943
Latino: 44.8 (16.5)
White: 28.3 (6.4)
Latino: 253,821
Black: 48.8 (17.5)
Black: 30.9 (7.5)
Latino: 14.0
Black: 135,934
Latino: 29.7 (6.4)
Black: 13.7
Incidence rate (per 1,000 person-years)
Korean: 20.3
South Asian: 17.2
Filipino: 14.7
SE Asian: 11.4
Japanese: 7.5
Chinese: 6.5
Vietnamese: 4.6
White: 6.3
Latino: 11.2
Black: 11.2
Wander et al., 2013 (36)
Japanese-American Community Diabetes Study Seattle, WA
421 Japanese Americans, 54% male
51.4 years (34.0–75.1)
Baseline
2-h 75-g OGTT
Cumulative incidence
Mean: 24.1 (range 16.6–36.9)
20.4%
After 5 years
5-year incidence
Incident T2D: 24.9
9.3%
Nondiabetic: 24.0
10-year incidence
Follow-up: 10 years
After 10 years
17.6%
Incident T2D: 25.4
Nondiabetic: 23.8
Chiu et al., 2011 (31)
Multiethnic Cohort Ontario Study
South Asian: 1,001
South Asian: 42 (36–49)
Self-reported BMI at baseline
Linkage with Ontario diabetes database (from multiple administrative sources)
Incidence rate (per 1,000 person-years)
Ontario, Canada
Chinese: 866
Chinese: 42 (36–50)
South Asian: 24.6 (22–27)
Baseline BMI 18.5–23
Mean follow-up: 12.8 years (1996–2009)
White: 57,210
White: 46 (38–57)
Chinese: 22.6 (20.0–24.0)
White: 3.1 (2.7–3.6)
Black: 747
Black: 42 (36–51)
White: 26.1 (23.0–28.0)
South Asian: 11.6 (6.0–17.8)
Black: 26.1 (23.0–28.0)
Chinese: 3.7 (1.1–6.4)
Black: 7.3 (1.1–16.9)
Baseline BMI 23–27.5
White: 6.9 (6.4–7.6)
South Asian: 20.2 (13.1–27.8)
Chinese: 16.8 (8.4–25.2)
Black: 14.1 (8.6–20.2)
Baseline BMI ≥27.5
White: 19.0 (17.9–20.0)
South Asian: 44.9 (28.1–63.9)
Chinese: 30.9 (10.9–52.6)
Black: 28.9 (17.0–42.9)
Maskarinec et al., 2009 (32)
Hawaii Component of the Multiethnic Cohort
Caucasian: 35,042
% in age category
% in BMI category
Insurance data, blood test
Incidence rate (per 1,000 person-years)
Hawaii
Japanese: 44,513
Japanese men
Japanese men
White: 5.8 (5.0–6.6)
Mean follow-up: 12 years
Hawaiian: 14,346
<55: 29.6%
BMI <22: 18.5%
Japanese: 12.5 (11.4–13.5)
Other: 9,997
55–64: 27.5%
BMI 22–24.9: 37.2%
Hawaiian: 15.5 (13.3–17.6)
≥65: 42.9%
BMI 25–29.9: 37.2%
Other: 12.2 (9.9–14.4)
Japanese women
BMI ≥30: 7.2%
<55: 29.9%
Japanese women
55–64: 29.6%
BMI <22: 41.5%
≥65: 40.5%
BMI 22–24.9: 29.7%
White men
BMI 25–29.9: 22.6%
<55: 42.6%
BMI ≥30: 6.2%
55–64: 27.6%
White men
≥65: 29.8%
BMI <22.0: 13.8%
White women
BMI 22.0–24.9: 31.6%
<55: 44.4%
BMI 25.0–29.9: 40.7%
55–64: 26.9%
BMI ≥30.0: 13.9%
≥65: 28.7%
White women
BMI <22: 33.2%
BMI 22.0–24.9: 27.4%
BMI 25.0–29.9: 25.2%
BMI ≥30.0: 14.1%
Data are mean (SD) unless otherwise indicated. FPG, fasting plasma glucose; SE, Southeast;
T2D, type 2 diabetes.
*
Self-reported Chinese, Indo-Chinese, Japanese, Korean, Pacific Islander, and Vietnamese.
Aggregated Data
The Women’s Health Initiative (28) enrolled postmenopausal women aged 50–79 years
from 40 clinical centers nationwide from 1993 to 1998 and followed them for 10.4 years.
Participants included 14,618 African American, 133,541 non-Hispanic white, 6,484 Latino/Hispanic,
and 4,190 Asian American women. Although the Asian American women self-reported as
being Chinese, Indo-Chinese, Japanese, Korean, Pacific Islander, or Vietnamese, data
were not disaggregated into these separate ethnic groups.
Baseline BMI was measured at the clinic visit, and incident diabetes was based on
self-reported affirmative responses that a doctor prescribed “pills for diabetes”
or “insulin shots for diabetes, collected at annual follow-up visits.” As shown in
Table 1, mean baseline BMI among Asians was 24.8 kg/m2, cumulative diabetes incidence
was 10.6%, and the incidence rate was 1.13 per 100 person-years. Compared with non-Hispanic
whites, Asian Americans had the highest risk for incident diabetes after adjusting
for age, study arm, baseline BMI, physical activity, dietary quality, smoking status,
family history of diabetes, and educational attainment (hazard ratio [HR] 1.86 [95%
CI 1.68−2.06]).
Disaggregated Data
The Diabetes Study of Northern California (DISTANCE) from Kaiser Permanente Northern
California (29), a large integrated health-delivery system, was a prospective study
in which enrolled adults were followed for 1 year. Data were disaggregated into 12
single racial/ethnic groups, including 7 distinct Asian subgroups. Of the 1,912,916
individuals without prevalent diabetes in 2010, a total of 15,357 incident diabetes
cases were identified in the following year. The incidence rates for diabetes were
highest among Pacific Islanders (19.9/1,000 person-years), followed by South Asians
(17.2), and Filipinos (14.7). The mean BMI at diagnosis among those who developed
incident diabetes was 27.2 kg/m2 in Chinese, 28.7 kg/m2 in Japanese, 29.0 kg/m2 in
Filipinos, and 29.6 kg/m2 in South Asians, compared with a mean BMI of 33.4 kg/m2
in non-Hispanic whites, 35.5 kg/m2 in African Americans, and 34.3 kg/m2 in Latinos
(A. Karter, personal communication). There was a consistent pattern across all racial/ethnic
groups of lower BMIs among individuals with prevalent diabetes when compared with
those with incident diabetes. Those with normal glucose levels had even lower BMI
compared with prevalent or incident diabetes cases. However, in other prospective
studies discussed in this section, the BMI used for analyses was collected at baseline
and may have preceded diabetes diagnosis by 5–10 years, depending on the duration
of study follow-up (28,30–32).
The Seattle Japanese-American Community Diabetes Study, conducted in King County,
WA, was a community-based prospective study of type 2 diabetes in second- and third-generation
adults of 100% Japanese ancestry in Seattle. This research has yielded many publications
on the relationship between body weight and body fat distribution, as well as the
prevalence and incidence of type 2 diabetes (33). Although publications from the Japanese-American
Community Diabetes Study have repeatedly shown the importance of central and especially
visceral fat as a risk factor for coronary heart disease (20), hypertension (34),
impaired glucose tolerance (35), type 2 diabetes (36), metabolic syndrome (37), and
insulin resistance (11), investigators also identified a relationship between BMI
and diabetes incidence when BMI was the sole measurement of body fat examined (38).
Among 466 nondiabetic Japanese Americans with a mean BMI 24.1 ± 0.2 kg/m2 at baseline,
49 developed diabetes at 5 years, based on a 75-g OGTT (30). Study participants who
developed diabetes had a mean BMI of 24.9 ± 0.5 kg/m2, while those remaining nondiabetic
had a mean BMI of 24.0 ± 0.2 kg/m2. These differences approached statistical significance
(P = 0.068). However, among participants aged ≤55 years, men who developed diabetes
were heavier than nondiabetic individuals, with mean respective BMIs of 28.7 ± 0.8
and 25.1 ± 0.3 kg/m2 (P < 0.001), while the difference in women (25.1 ± 1.2 and 22.8
± 0.3 kg/m2) did not reach statistical significance. Among men or women aged >55 years,
incident diabetes was not associated with baseline BMI. In participants ≤55 years
of age, the 5-year relative risk of diabetes associated with BMI was 26.5 (95% CI
3.4−204) but was 0.8 (95% CI 0.4−1.7) for those >55 years of age. Thus in this analysis
at 5 years, BMI predicted risk for diabetes in Japanese Americans ≤55 years of age
but not in those >55 years of age.
In a subsequent analysis of 424 initially nondiabetic Japanese Americans who were
followed for additional 5 years (total of 10 years), 74 developed diabetes (36). Those
developing diabetes had a mean BMI of 25.4 ± 3.7 kg/m2, while those who remained nondiabetic
had a mean BMI of 23.8 ± 3.1 kg/m2. The odds of incident diabetes for a 1 SD increase
in BMI were 1.57 (95% CI 1.23−2.02). Thus, these two studies indicate that BMI is
a significant risk factor for incident diabetes in Japanese Americans and that the
BMI levels at which diabetes develops are quite low. However, neither report provided
an inflection point for BMI at which risk was significantly increased.
A multiethnic cohort study identified nondiabetic adults in Ontario, Canada, using
Statistics Canada’s 1996 National Population Health Survey and the Canadian Community
Health Survey (31). Survey participants living in Ontario, aged ≥30 years at the time
of survey, and who self-reported as South Asian (n = 1,001) or Chinese (n = 866) comprised
the Asian cohorts and were followed for a median of 6 years. Also included were blacks
(n = 747) and non-Hispanic whites (n = 57,210). BMI was based on self-reported weight
and height at baseline, and incident diabetes cases were ascertained through record
linkage with the population-based Ontario Diabetes Database using a validated administrative
data algorithm. Participants were followed from the survey interview date to the date
of diabetes diagnosis, death, or at the end of the study. At baseline, mean BMI was
24.6 kg/m2 among South Asians, 22.6 kg/m2 among Chinese, 26.1 kg/m2 among blacks,
and 26.1 kg/m2 among non-Hispanic whites. Researchers found that incident diabetes
risk, adjusted for age, sex, sociodemographic characteristics, and BMI, was significantly
higher for South Asians (20.8/1,000 person-years; HR 3.40), blacks (16.3/1,000; 1.99),
and Chinese (9.3/1,000; 1.87), compared with non-Hispanic whites (9.5/1,000). The
BMI cutoff value at which diabetes incidence was equivalent to BMI 30 kg/m2 for non-Hispanic
whites was estimated at 24 kg/m2 for South Asians, 25 kg/m2 for Chinese, and 26 kg/m2
for blacks. Additionally, the median age at diagnosis was younger for South Asians
(49 years) and Chinese (55 years) compared with blacks (57 years) and non-Hispanic
whites (58 years).
Last, the Multiethnic Cohort (32) in Hawaii included non-Hispanic whites, Native Hawaiians,
and Japanese Americans. The Hawaii data from this cohort were linked to two diabetes
care registries (Blue Cross/Blue Shield and Kaiser Permanente Hawaii). Incident type
2 diabetes was identified by self-report of medical conditions between 1999 and 2003,
a medication questionnaire, and linkage with health insurance plans in 2007. Native
Hawaiians had the highest incidence (15.5/1,000 person-years), followed by Japanese
Americans (12.5/1,000), while non-Hispanic whites had the lowest incidence (5.8 cases/1,000).
The authors compared the HR of incident diabetes at different BMI cut points for each
racial/ethnic group and found that Japanese Americans had a significantly higher incidence
of diabetes at BMI 22.0–24.9 kg/m2 than Hawaiians or non-Hispanic whites. Diabetes
risk for Japanese Americans was higher than for non-Hispanic whites at all BMI levels.
Even at BMI cut points of <22 kg/m2 and 22.0−24.9 kg/m2, respectively, HRs were higher
among Japanese Americans compared with non-Hispanic whites at BMI cut points of 25.0−29.9
kg/m2.
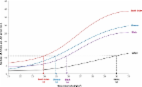
New Cross-sectional Analysis
Most recently, in an effort to ascertain the lowest BMI cut point that might be practical
for identifying Asian American adults (aged ≥45 years) with previously undiagnosed
type 2 diabetes, a group of investigators presented a new analysis at the 2014 Scientific
Sessions of the American Diabetes Association (ADA) based on combined data from four
cohort studies (39).The data set included participants without a prior diabetes diagnosis,
aged ≥45 years, with no non-Asian admixture. Participant data were obtained from the
University of California San Diego Filipino Health Study, San Diego, CA (n = 421);
North Kohala Study, Hawaii, HI (n = 115 Filipinos, 129 Japanese, 18 other Asian);
Seattle Japanese-American Community Diabetes Study, Seattle, WA (n = 371); and the
Mediators of Atherosclerosis in South Asians Living in America (MASALA), San Francisco,
CA, and Chicago, IL (n = 609). All 1,663 participants underwent 2-h 75-g OGTT, and
diabetes diagnosis was based on ADA 2014 criteria (40). In the total sample, a BMI
≥26 kg/m2 cut point had the lowest misclassification rate (false-positive + false-negative
rates) and highest Youden’s index (sensitivity + specificity −1). Sensitivity approximated
specificity at BMI ≥25.4 kg/m2; however, limiting screening at BMI ≥25 kg/m2 would
miss 36% of Asian Americans with newly diagnosed type 2 diabetes. In the same study,
Araneta et al. (39) found that screening Asian Americans at a BMI cut point of ≥23.5
kg/m2 identified approximately 80% of those with undiagnosed type 2 diabetes. Among
Japanese Americans, lowering the BMI screening cut point to ≥22.8 kg/m2 achieved 80%
sensitivity. The same study also showed that limiting screening to HbA1c ≥6.5% fails
to identify almost half of Asian Americans with diabetes and 44% who had isolated
postchallenge hyperglycemia would be missed without an OGTT.
Conclusions
This comprehensive review and analysis of the association between BMI and diabetes
in Asian Americans illustrates that Asian Americans have a higher prevalence of type
2 diabetes at relatively lower BMI cut points than whites. Given that established
BMI cut points indicating elevated diabetes risk are inappropriate for Asian Americans,
establishing a specific BMI cut point to identify Asian Americans with or at risk
for future diabetes would be beneficial to the potential health of millions of Asian
American individuals.
Generally, the rationale behind the conventional BMI cut point has been the observation
that overweight and obese adults (18 years of age or older) with a BMI of ≥25 kg/m2
have increased risks of both morbidity and mortality. Adults who meet or exceed the
25 kg/m2 BMI threshold are at increased risk of developing coronary heart disease,
hypertension, hypercholesterolemia, type 2 diabetes, and other diseases, in addition
to showing increases in mortality (41). However, while the studies reviewed herein
do indicate increased diabetes prevalence among Asian Americans with BMIs below the
25 kg/m2 threshold, a recent study (42) found no evidence to suggest an increased
risk of total mortality among Asian Americans within the BMI range of 20 to <25 kg/m2.
Therefore, it is important to note that the aim of this position statement is not
to redefine BMI cut points that constitute overweight and obesity thresholds as they
relate to mortality or morbidity in Asian Americans. Instead, the intent is to clarify
how to use BMI as a simple initial screening tool to identify Asian Americans who
may have diabetes or be at risk for future diabetes. The question being considered
is the most appropriate BMI cut point indicative of elevated risk of diabetes in Asian
Americans. Historically, there has been a general acknowledgment that a BMI cutoff
point lower than 25 kg/m2 would increase the likelihood of identifying diabetes or
diabetes risk in Asians. Thus in the Diabetes Prevention Program (DPP), a BMI value
of 22 kg/m2 was selected as the eligibility BMI for Asians (43). The 2014 ADA “Standards
of Medical Care in Diabetes” (40) indicates that there is compelling evidence that
lower BMI cut points, specifically BMI cutoff value of 24 kg/m2 in South Asians and
25 kg/m2 in Chinese, denote increased diabetes risk in some racial and ethnic groups,
although the ADA Standards fall short of identifying an exact cut point. However in
2000, a group cosponsored jointly by the Regional Office for the Western Pacific (WPRO)
of the World Health Organization, the International Association for the Study of Obesity,
and the International Obesity Task Force published in an extensive monograph a recommendation
that the BMI value to denote overweight in Asians should be ≥23 kg/m2 and ≥25 kg/m2
for obesity (44). Subsequently, the World Health Organization consultation group identified
potential public health action points along the BMI continuum ranging from 23.0 to
27.5 kg/m2 and proposed that each country make decisions regarding the definitions
of increased risk for its population (45). They did not identify an exact cut point.
In addition, some Asian countries have taken steps to set new BMI obesity cut points
for their populations. In 1992, the Japan Society for the Study of Obesity (JASSO)
decided to define BMI ≥25 kg/m2 as obesity (46). In China, a BMI of 24 kg/m2 was found
to have the best sensitivity and specificity for risk-factor identification and was
recommended as the cutoff point for overweight. A BMI of 28 kg/m2 was found to identify
risk factors with specificity approximately 90% and was recommended as the cutoff
point for obesity (47). Likewise, the diagnostic cutoff for overweight BMI in India
(48) is 23 kg/m2.
Determining the optimal BMI cut point for identifying Asian Americans at elevated
risk for diabetes is complex. There is tremendous heterogeneity among the Asian American
subgroups. For example, data from the DISTANCE study might suggest a conventional
BMI cut point of 25 kg/m2 as an acceptable threshold (29), especially for South Asians
and Southeast Asians. In contrast, the Women’s Health Initiative (28), the Seattle
Japanese-American Community Diabetes Study (36), the multiethnic cohort study from
Canada (31), and the Multiethnic Cohort in Hawaii (32) would lend support to lowering
the BMI cut point, especially for East Asians (Chinese and Japanese).
In light of the diabetes epidemic, there is an urgent need to increase early detection
and activate the at-risk public toward diabetes prevention. Adopting a single lower
and uniform BMI cut point for Asian Americans would serve to increase opportunities
for education, intervention, behavior and lifestyle change, and diagnosis. In support
of this approach, data from Araneta et al. (39) suggest that for diabetes screening
purposes BMI cut points with a sensitivity of 80% fall consistently between 23–24
kg/m2 for nearly all Asian American subgroups (with levels slightly lower for Japanese).
This makes a rounded cut point of 23 kg/m2 practical. In determining a single BMI
cut point, it is important to balance sensitivity and specificity so as to provide
a valuable screening tool without numerous false positives. Furthermore, for a screening
tool to be most valuable, it must be at least as useful as other commonly available
tools. A BMI cut point of 23 kg/m2 will have greater sensitivity than the ADA general
screening questionnaire’s (ADA Type 2 Diabetes Risk Test) sensitivity of 70–80% (49).
An argument can be made to push the BMI cut point to lower than 23 kg/m2 in favor
of even further increased sensitivity. However, this would lead to an unacceptably
low specificity (13.1%) (39).
The authors of this position statement propose that the analysis of BMI and diabetes
in Asian Americans and subsequent recommendation of an Asian American−specific BMI
cut point of 23 kg/m2 for diabetes screening in the U.S. have the advantage of being
predicated on available data for Asian Americans, not Asian country data. In this
way, this recommendation takes into consideration not only genetic and physiologic
factors but also environmental and lifestyle context. Further, it is based on a comprehensive
review of available literature with focus on longitudinal studies and includes data
from several large Asian American subgroups.
However, the analysis is limited in several ways. First, no uniform method of diagnosis
was used in the studies upon which this recommendation is based. Diagnostic methods
ranged from medication usage data, self-report, HbA1c, fasting blood glucose, and
OGTT. Studies using diagnostic methods other than OGTT might have understated diabetes
prevalence (20–22,39). Second, some studies were not based on BMI data available at
the time of incident diabetes. Rather, most studies reported the association between
baseline BMI and diabetes diagnosis, with these measurements as much as 5–10 years
apart in some instances. Therefore, these data do not accurately reflect the relationship
of BMI to diabetes diagnosis at the time of diagnosis. Third, the number of robust
studies is limited. Additional research will help to further elucidate current findings
on the relationship between BMI and incident diabetes in Asian Americans. Fourth,
while some data exist for several Asian ethnic subgroups, insufficient disaggregated
data are available for many of the Asian ethnic groups that comprise this very heterogeneous
population.
Much is known about how to prevent diabetes for those at risk (primary prevention)
and about how to prevent or reduce complications in those with diabetes (secondary
prevention). Diabetes is no longer the same life-threatening, life-limiting condition
it was a century or even several decades ago. However, without increased prevention
and early diagnosis the benefits of these strategies will not be fully realized. Because
Asian Americans’ risk for diabetes is under-recognized based on the existing BMI criteria,
this population may not be afforded the same opportunity as others for increased prevention
and early diagnosis. It is imperative to better screen and diagnose America’s fastest-growing
ethnic group based on the BMI cut point that more appropriately applies to them. While
more research is needed to identify better risk markers than BMI and future research
efforts will undoubtedly bring us closer to understanding the metabolic profiles of
specific ethnic subgroups, with the subsequent development of appropriate personalized
medicine, there is an urgent need for action now, even in the absence of perfect data.
ADA Recommendation
Testing for diabetes should be considered for all Asian American adults who present
with a BMI of ≥23 kg/m2.
Related collections
Most cited references32
- Record: found
- Abstract: found
- Article: not found
Waist circumference and abdominal sagittal diameter: best simple anthropometric indexes of abdominal visceral adipose tissue accumulation and related cardiovascular risk in men and women.
M Pouliot, J P Després, S Lemieux … (1994)
- Record: found
- Abstract: found
- Article: found
Deriving Ethnic-Specific BMI Cutoff Points for Assessing Diabetes Risk
Maria Chiu, Peter C Austin, Douglas G. Manuel … (2011)
- Record: found
- Abstract: found
- Article: not found
Impaired glucose tolerance and impaired fasting glycaemia: the current status on definition and intervention.
Daniel Shaw, K Alberti, N Unwin … (2002)
