- Record: found
- Abstract: found
- Article: found
Split-Rib Cranioplasty Using a Patient-Specific Three-Dimensional Printing Model
case-report
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
The reconstruction of cranial bone defects is necessary not just for the protection
of the brain, but also for aesthetics. Cranial bone reconstruction may be conducted
using autologous or synthetic bone tissue [1]. When synthetic bone is utilized, the
reconstruction of large defects is possible, and problems with the donor area are
eliminated. However, other possible problems include allergic reaction, infection,
and implant exposure [2]. The reconstruction of cranial bone defects using autologous
bone tissue has the advantages of avoiding both allergic reaction and implant exposure,
but potential problems include donor site morbidity, prolonged surgical time, unpredictable
resorption, and asymmetrical bone shape [3
4]. The advantages and disadvantages of these two methods complement each other.
With the development of three-dimensional printing (3D printing) technology, the prefabrication
of patient-specific implants is now helping to achieve a symmetrical cranial shape,
and minimize tissue damage [5]. While surgical methods utilizing the latest in 3D
printing technology have proven to be a great help in producing alloplastic material
for cranioplasty, to the author's knowledge, there have been no reports of surgery
using 3D printing for methods of grafting autologous bone tissue. Accordingly, by
conducting autologous cranioplasty using 3D printing, the authors obtained favorable
results both functionally and aesthetically, which are presented here.
A sixteen-year-old patient who had suffered cerebral hemorrhage after being injured
in a traffic accident underwent a two-stage extensive decompressive craniectomy. One
area was reconstructed using preserved bone fragments, but in another area, in which
the bone fragments had not been preserved, a 14 cm×12 cm skull defect remained (Fig.
1). Considering the fact that the patient was very active and was comparatively young,
a plan was devised to perform a split-rib autologous graft. In order to harvest the
portion of rib bone with precisely matching curvature, a rib and skull model was printed
from preoperative 3D-computed tomography (CT) scans of the patient using 3D printing
technology (Fig. 2). The machine used for 3D printing in this study's case was 3D
Systems ProJet 660Pro. This is not a model constructed for medical use, but rather
a machine used mainly for the making of ordinary commercial test products. After simple
conversion of the filename extension of the CT image file, a patient-specific 3D model
was printed. The printed model was used to compare the skull defect with the shape
of the ribs, and a design was preoperatively marked on a portion of the right seventh
and ninth ribs, the most ideal graft candidates (Fig. 3). Afterwards, there was a
need to select a landmark in order to excise a portion of rib bone that precisely
matched the bone portion simulated in the operating room. While the sternocostal joint
and costochondral junction are commonly used as landmarks for rib bones, we could
not use them as landmarks because cartilage is not printed in a bone 3D printing model.
However, the seventh and ninth ribs have considerably long cartilage, so it is impossible
to find this part in the patient's body by exploration with the fingers. An important
landmark that we used was the highest point of the seventh and ninth ribs in a lateral
position. We calculated the distance from this point to the front and back side of
the rib bone to be excised, and after marking the area to be excised on the skin.
Then, we performed infiltration with an ink-filled syringe and marked the precise
excision area up to the area adjacent to the bone. After this, the periosteal layer
on the rib was elevated, exposing the bony portions of the rib as designed, and minimal
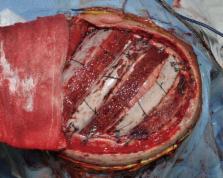
bone harvesting was accomplished. The harvested ribs were split in two. Reconstruction
of the skull bone defect was then conducted using the split-rib bone graft as simulated
(Fig. 4). After surgery, the cranioplasty was successful, and none of the cases experienced
respiratory problems. The patients nearly reached aesthetic symmetry (Fig. 5).
In cases such as the one in this study where the defect size is large, the precise
amount and portion of the rib to be resected must be determined. The current method
of only using 3D-CT images has the limitation of depending on a visual estimation,
and thus the amount of rib to be resected must be larger than the size of the defect,
which can lead to donor site complications, and pneumothorax is also a risk. Besides,
there is also a great possibility that reconstruction will not be aesthetically satisfactory
due to a difference in the curvature of the rib and the skull. Cranioplasty utilizing
synthetic materials has the advantage of not causing donor site complications, as
well as being able to achieve perfect symmetry through the creation of patient-specific
implants using 3D printing. However, there are potential complications with this procedure,
including infection and allergic reaction, and its use should definitely be avoided
in the case of children, whose bones have not yet stopped growing. In the case of
the sixteen-year-old patient in this study, while alloplastic cranioplasty was possible,
as the growth of the skull bone was nearly complete, the patient and his guardian
decided upon autologous cranioplasty. In cases of large autologous cranioplasty, such
as the one reported in this study, using a patient-specific 3D model as a preoperative
procedure can have several advantages. First, donor site complications can be reduced
by performing a simulated operation using the 3D model in advance. Respiratory complications
that can occur in split-rib cranioplasty can also be reduced with minimal rib resection.
Second, aesthetically satisfactory results can be achieved. If resection is performed
after preoperatively determining the ideal rib portion that best matches the defect's
curvature through a 3D model, the surgeon can find the ideal portion of rib bone that
will cover the skull defect.
Medical limitations can be overcome when new technology is introduced. Rapid advances
in 3D printing technology have positively affected its application in the field of
cosmetic surgery. Using various patient-specific 3D models in alloplastic cranioplasty
addresses a number of limitations for various procedures. However, the application
of 3D printing technology in autologous cranioplasty is limited. This study reports
notable results when a 3D printing model is utilized in autologous cranioplasty. Further
studies are needed to verify the effectiveness of 3D printing technology in autologous
cranioplasty.
Related collections
Most cited references5

- Record: found
- Abstract: found
- Article: found
Cranioplasty: Review of materials and techniques
Seckin Aydin, Baris Kucukyuruk, Bashar Abuzayed … (2011)
- Record: found
- Abstract: found
- Article: not found
Clinical outcome in cranioplasty: critical review in long-term follow-up.
Andrea Moreira, Vincent DiNick, Khaled Barakat … (2003)
- Record: found
- Abstract: found
- Article: not found
The use of frozen autogenous bone flaps in delayed cranioplasty revisited.
Toru Iwama, Jun Yamada, Syu Imai … (2003)
Author and article information
Comments
Comment on this article
scite_
8
0
9
0
 Smart Citations
Smart Citations8
0
9
0
Citing PublicationsSupportingMentioningContrasting
See how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.