- Record: found
- Abstract: found
- Article: found
Effectiveness of eHealth Interventions and Information Needs in Palliative Care: A Systematic Literature Review
Abstract
Background
One of the key components in palliative care is communication. eHealth technologies can be an effective way to support communications among participants in the process of palliative care. However, it is unclear to what extent information technology has been established in this field.
Objective
Our goal was to systematically identify studies and analyze the effectiveness of eHealth interventions in palliative care and the information needs of people involved in the palliative care process.
Methods
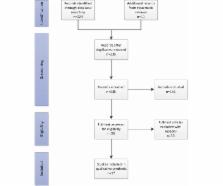
We conducted a systematic literature search using PubMed, Embase, and LILACS according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. We collected and analyzed quantitative and qualitative data regarding effectiveness of eHealth interventions and users’ information needs in palliative care.
Results
Our search returned a total of 240 articles, 17 of which met our inclusion criteria. We found no randomized controlled trial studying the effects of eHealth interventions in palliative care. Studies tended to be observational, noncontrolled studies, and a few quasi-experimental studies. Overall there was great heterogeneity in the types of interventions and outcome assessments; some studies reported some improvement on quality of care, documentation effort, cost, and communications. The most frequently reported information need concerned pain management.
Related collections
Most cited references24
- Record: found
- Abstract: not found
- Article: not found
Palliative Care: the World Health Organization's global perspective.
- Record: found
- Abstract: found
- Article: not found
Overcoming Depression on the Internet (ODIN) (2): A Randomized Trial of a Self-Help Depression Skills Program With Reminders
- Record: found
- Abstract: found
- Article: not found