- Record: found
- Abstract: found
- Article: not found
Colorectal Surgery Outcomes in the United States during the COVID-19 Pandemic
Read this article at
Abstract
Background
The purpose of this study was to assess colorectal surgery outcomes, discharge destination, and readmission in the United States during the COVID-19 pandemic.
Methods
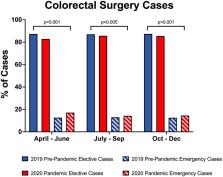
Adult colorectal surgery patients in the American College of Surgeons National Surgical Quality Improvement Program database (2019-2020) and its colectomy and proctectomy procedure-targeted files were included. The pre-pandemic time period was defined from April 1, 2019-December 31, 2019. The pandemic time period was defined from April 1, 2020-December 31, 2020 in quarterly intervals (Q2 April-June; Q3 July-September; Q4 October-December). Factors associated with morbidity and in-hospital mortality were assessed using multivariable logistic regression.
Results
Among 62,393 patients, 34,810 patients (55.8%) underwent colorectal surgery pre-pandemic, and 27,583 (44.2%) during the pandemic. Patients who had surgery during the pandemic had higher American Society of Anesthesiologists class and presented more frequently with dependent functional status. The proportion of emergent surgeries increased (12.7% pre-pandemic vs. 15.2% pandemic, p<0.001), with fewer laparoscopic cases (54.0% vs. 51.0%, p<0.001). Higher rates of morbidity with a greater proportion of discharges to home and lesser proportion of discharges to skilled care facilities were observed with no considerable differences in length of stay or worsening readmission rates. Multivariable analysis demonstrated increased odds of overall and serious morbidity, as well as in-hospital mortality, during Q3 and/or Q4 of the 2020 pandemic.
Conclusions
Differences in hospital presentation, inpatient care, and discharge disposition of colorectal surgery patients were observed during the COVID-19 pandemic. Pandemic responses should emphasize balancing resource allocation, educating patients and providers on timely medical workup and management, and optimizing discharge coordination pathways.
Related collections
Most cited references27
- Record: found
- Abstract: found
- Article: not found
Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey.
- Record: found
- Abstract: found
- Article: found
Factors Associated With Surgical Mortality and Complications Among Patients With and Without Coronavirus Disease 2019 (COVID-19) in Italy
- Record: found
- Abstract: found
- Article: not found
