- Record: found
- Abstract: found
- Article: found
Subcutaneous Direct-to-Implant Breast Reconstruction: Surgical, Functional, and Aesthetic Results after Long-Term Follow-Up
Read this article at
Abstract
Supplemental Digital Content is available in the text.
Abstract
Background:
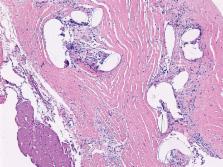
Direct-to-implant breast reconstruction can be achieved more easily by means of soft-tissue replacement devices such as dermal matrices and synthetic meshes. The feasibility of a subcutaneous approach has been recently investigated by some studies with different devices functioning as implant support. Aim of this study is to analyze the long-term results, both objective and subjective, of a previous nonrandomized trial comparing prepectoral (subcutaneous) and retropectoral breast reconstructions.
Methods:
Patients enrolled in a nonrandomized prospective trial, comparing the standard retropectoral reconstruction and the prepectoral subcutaneous approach, using a titanium-coated mesh in both techniques, were followed up and evaluated for long-term results. Cases were compared in terms of the causes and rate of reinterventions, of the postoperative BREAST-Q questionnaire results, and of an objective surgical evaluation.
Results:
The subcutaneous group had a rate of implant failure and removal of 5.1% when compared with 0% in the retropectoral group. Aesthetic outcome was significantly better for the subcutaneous group both at a subjective and at an objective evaluation. Capsular contracture rate was 0% in the subcutaneous group.
Conclusions:
A higher rate of implant failure and removal, although not significant, always because of skin flaps and wound problems, should be taken into account for a careful patients selection. The subcutaneous breast reconstruction shows good long-term results. A coherent subjective and objective cosmetic advantage of this approach emerges. Moreover, no capsular contracture is evident, albeit in a relatively limited number of cases.
Related collections
Most cited references29
- Record: found
- Abstract: found
- Article: not found
Implant-based breast reconstruction using acellular dermal matrix and the risk of postoperative complications.
- Record: found
- Abstract: found
- Article: not found
A meta-analysis of human acellular dermis and submuscular tissue expander breast reconstruction.
- Record: found
- Abstract: found
- Article: not found