- Record: found
- Abstract: found
- Article: found
EMPHYSEMATOUS PYELONEPHRITIS
letter
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
Dear Editor,
A 48-year-old female with poorly controlled diabetes mellitus (DM) presented herself
with a five-day history of fever, chills, left flank pain and dysuria. On
admission, her abdomen was mildly distended and tender over the left lumbar
region. Laboratory data showed white blood cell count of 18.6×109/L
with 91.7% neutrophils, serum creatinine at 223 μmol/L, C-reactive protein at 168
mg/L and glycosylated hemoglobin (HbA1c) at 14.1%. Urine analysis showed turbid
appearance with obvious pyuria, hematuria and proteinuria. A renal ultrasound scan
revealed potential signs of gas in the parenchyma of the left kidney. A
non-contrast computed tomography (CT) scan of the abdomen demonstrated swelling of
the left kidney with visible gas in the renal parenchyma (Fig. 1), radiologically
associated with emphysematous
pyelonephritis (EPN, Class 2). The patient underwent CT-guided percutaneous
catheter drainage (PCD) and was treated with broad-spectrum intravenous
antibiotics and rigorous blood sugar control. The urine and pus cultures showed
significant growth of Escherichia coli (E.
coli). From the above medical procedures, the patient improved
significantly and was discharged with an excellent prognosis.
EPN is an uncommon, but acutely severe and life-threatening necrotizing kidney
infection, which is characterized by gas accumulation
in the renal parenchyma, collecting system, or perinephric tissue1
,
2
,
4. The disease usually occurs in female
patients with poorly controlled DM, with or without urinary tract obstruction1
,
2
,
4. E. coli is the most
common pathogen, which has been extracted from urine or pus cultures in almost 70%
of the patients4. EPN is a radiological
diagnosis, with CT scan currently being the imaging procedure of choice for early
diagnosis and assessment of the disease1
,
2
,
4. Importantly, PCD is now the most
appropriate strategy and the gold standard in management of EPN2
,
3. Over the last two decades, improvements
in management techniques have drastically reduced the mortality rate of EPN to
21%3
,
4.
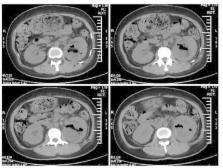
Fig. 1
Computed tomography (CT) scan of the abdomen showing a mottled
gas collection within the parenchyma of the swelling left
kidney
Related collections
Most cited references5
- Record: found
- Abstract: found
- Article: not found
Emphysematous pyelonephritis: clinicoradiological classification, management, prognosis, and pathogenesis.
J. -J. Huang, C Tseng (2000)
- Record: found
- Abstract: found
- Article: not found
Emphysematous pyelonephritis.
Sarvpreet Ubee, Laura McGlynn, Mark V.P. Fordham (2011)
- Record: found
- Abstract: found
- Article: not found
Is percutaneous drainage the new gold standard in the management of emphysematous pyelonephritis? Evidence from a systematic review.
Bhaskar K. Somani, Ghulam Nabi, Peter Thorpe … (2008)