- Record: found
- Abstract: found
- Article: found
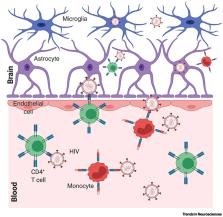
The Paradox of HIV Blood–Brain Barrier Penetrance and Antiretroviral Drug Delivery Deficiencies
Read this article at
Abstract
HIV attacks the body’s immune cells, frequently compromises the integrity of the blood–brain barrier (BBB), and infects the CNS in the early stages of infection. Dysfunction of the BBB further potentiates viral replication within the CNS, which can lead to HIV-associated neuropathology. Antiretroviral therapy (ART) significantly improves HIV patient outcomes and reduces mortality rates. However, there has been limited progress in targeting latent viral reservoirs within the CNS, which may eventually lead to rebound viremia. While ART drugs are shown to be effective in attenuating HIV replication in the periphery, the protection of the brain by the BBB offers an isolated sanctuary to harbor HIV and maintains chronic and persistent replication within the CNS. In this review, we elucidate the pathology of the BBB, its ability to potentiate viral replication, as well as current therapies and insufficiencies in treating HIV-infected individuals.
Related collections
Most cited references81
- Record: found
- Abstract: found
- Article: not found
Nanoparticle-based targeted drug delivery.
- Record: found
- Abstract: found
- Article: not found
A novel quantitative approach for measuring the reservoir of latent HIV-1 proviruses
- Record: found
- Abstract: found
- Article: not found