- Record: found
- Abstract: found
- Article: found
Overexpression of EphB2 in the basolateral amygdala is crucial for inducing visceral pain sensitization in rats subjected to water avoidance stress

Read this article at
Abstract
Aims
Basolateral amygdala (BLA), as a center for stress responses and emotional regulation, is involved in visceral hypersensitivity of irritable bowel syndrome (IBS) induced by stress. In the present study, we aimed to investigate the role of EphB2 receptor (EphB2) in BLA and explore the underlying mechanisms in this process.
Methods
Visceral hypersensitivity was induced by water avoidance stress (WAS). Elevated plus maze test, forced swimming test, and sucrose preference test were applied to assess anxiety‐ and depression‐like behaviors. Ibotenic acid or lentivirus was used to inactivate BLA in either the induction or maintenance stage of visceral hypersensitivity. The expression of protein was determined by quantitative PCR, immunofluorescence, and western blot.
Results
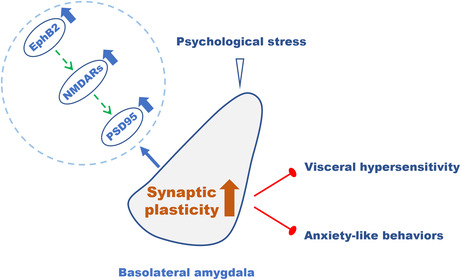
EphB2 expression was increased in BLA in WAS rats. Inactivation of BLA or downregulation of EphB2 in BLA failed to induce visceral hypersensitivity as well as anxiety‐like behaviors. However, during the maintenance stage of visceral pain, visceral hypersensitivity was only partially relieved but anxiety‐like behaviors were abolished by inactivation of BLA or downregulation of EphB2 in BLA. Chronic WAS increased the expression of EphB2, N‐methyl‐D‐aspartate receptors (NMDARs), and postsynaptic density protein (PSD95) in BLA. Downregulation of EphB2 in BLA reduced NMDARs and PSD95 expression in WAS rats. However, activation of NMDARs after the knockdown of EphB2 expression still triggered visceral hypersensitivity and anxiety‐like behaviors.
Conclusions
Taken together, the results suggest that EphB2 in BLA plays an essential role in inducing visceral hypersensitivity. In the maintenance stage, the involvement of EphB2 is crucial but not sufficient. The increase in EphB2 induced by WAS may enhance synaptic plasticity in BLA through upregulating NMDARs, which results in IBS‐like symptoms. These findings may give insight into the treatment of IBS and related psychological distress.
Abstract
Related collections
Most cited references66
- Record: found
- Abstract: found
- Article: not found
Central sensitization: implications for the diagnosis and treatment of pain.
- Record: found
- Abstract: found
- Article: not found
Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features and Rome IV.
- Record: found
- Abstract: found
- Article: not found