- Record: found
- Abstract: found
- Article: found
Patient and Operational Factors Do Not Substantively Affect the Annual Departmental Quality of Anesthesiologists’ Clinical Supervision and Nurse Anesthetists’ Work Habits
Read this article at
Abstract
Introduction: Although safety climate, teamwork, and other non-technical skills in operating rooms probably influence clinical outcomes, direct associations have not been shown, at least partially due to sample size considerations. We report data from a retrospective cohort of anesthesia evaluations that can simplify the design of prospective observational studies in this area. Associations between non-technical skills in anesthesia, specifically anesthesiologists’ quality of clinical supervision and nurse anesthetists’ work habits, and patient and operational factors were examined.
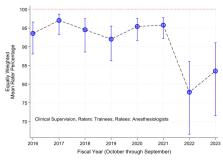
Methods: Eight fiscal years of evaluations and surgical cases from one hospital were included. Clinical supervision by anesthesiologists was evaluated daily using a nine-item scale. Work habits of nurse anesthetists were evaluated daily using a six-item scale. The dependent variables for both groups of staff were binary, whether all items were given the maximum score or not. Associations were tested with patient and operational variables for the entire day.
Results: There were 40,718 evaluations of faculty anesthesiologists by trainees, 53,772 evaluations of nurse anesthetists by anesthesiologists, and 296,449 cases that raters and ratees started together. Cohen’s d values were small (≤0.10) for all independent variables, suggesting a lack of any clinically meaningful association between patient and operational factors and evaluations given the maximum scores. For supervision quality, the day’s count of orthopedic cases was a significant predictor of scores (P = 0.0011). However, the resulting absolute marginal change in the percentage of supervision scores equal to the maximum was only 0.8% (99% confidence interval: 0.2% to 1.4%), i.e., too small to be of clinical or managerial importance. Neurosurgical cases may have been a significant predictor of work habits (P = 0.0054). However, the resulting marginal change in the percentage of work habits scores equal to the maximum, an increase of 0.8% (99% confidence interval: 0.1% to 1.6%), which was again too small to be important.
Conclusions: When evaluating the effect of assigning anesthesiologists and nurse anesthetists with different clinical performance quality on clinical outcomes, supervision quality and work habits scores may be included as independent variables without concern that their effects are confounded by association with the patient or case characteristics. Clinical supervision and work habits are measures of non-technical skills. Hence, these findings suggest that non-technical performance can be judged by observing the typical small sample size of cases. Then, associations can be tested with administrative data for a far greater number of patients because there is unlikely to be a confounding association between patient and case characteristics and the clinicians’ non-technical performance.
Related collections
Most cited references52
- Record: found
- Abstract: not found
- Article: not found
Technical Note: Review of methods for linear least-squares fitting of data and application to atmospheric chemistry problems
- Record: found
- Abstract: found
- Article: not found
Association Between Handover of Anesthesia Care and Adverse Postoperative Outcomes Among Patients Undergoing Major Surgery
- Record: found
- Abstract: found
- Article: not found