- Record: found
- Abstract: found
- Article: found
Evaluation of a Multichannel Non-Contact ECG System and Signal Quality Algorithms for Sleep Apnea Detection and Monitoring
Read this article at
Abstract
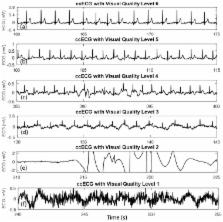
Sleep-related conditions require high-cost and low-comfort diagnosis at the hospital during one night or longer. To overcome this situation, this work aims to evaluate an unobtrusive monitoring technique for sleep apnea. This paper presents, for the first time, the evaluation of contactless capacitively-coupled electrocardiography (ccECG) signals for the extraction of sleep apnea features, together with a comparison of different signal quality indicators. A multichannel ccECG system is used to collect signals from 15 subjects in a sleep environment from different positions. Reference quality labels were assigned for every 30-s segment. Quality indicators were calculated, and their signal classification performance was evaluated. Features for the detection of sleep apnea were extracted from capacitive and reference signals. Sleep apnea features related to heart rate and heart rate variability achieved high similarity to the reference values, with p-values of 0.94 and 0.98, which is in line with the more than 95% beat-matching obtained. Features related to signal morphology presented lower similarity with the reference, although signal similarity metrics of correlation and coherence were relatively high. Quality-based automatic classification of the signals had a maximum accuracy of 91%. Best-performing quality indicators were based on template correlation and beat-detection. Results suggest that using unobtrusive cardiac signals for the automatic detection of sleep apnea can achieve similar performance as contact signals, and indicates clinical value of ccECG. Moreover, signal segments can automatically be classified by the proposed quality metrics as a pre-processing step. Including contactless respiration signals is likely to improve the performance and provide a complete unobtrusive cardiorespiratory monitoring solution; this is a promising alternative that will allow the screening of more patients with higher comfort, for a longer time, and at a reduced cost.
Related collections
Most cited references38
- Record: found
- Abstract: found
- Article: not found
Robust heart rate estimation from multiple asynchronous noisy sources using signal quality indices and a Kalman filter.
- Record: found
- Abstract: found
- Article: not found
Signal-quality indices for the electrocardiogram and photoplethysmogram: derivation and applications to wireless monitoring.
- Record: found
- Abstract: found
- Article: not found