- Record: found
- Abstract: found
- Article: found
Fungal Malignant Otitis Externa Involves a Cascade of Complications Culminating in Pseudoaneurysm of Internal Maxillary Artery: A Case Report
Read this article at
Abstract
Patient: Male, 66
Final Diagnosis: Pseudoaneurysm of internal maxillary artery secondary to fungal malignant otitis externa
Symptoms: Epistaxis
Medication: —
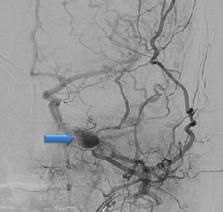
Clinical Procedure: Functional endoscopic sinus surgery, endovascular embolization
Specialty: Infectious Diseases
Background:
Pseudomonal infection is the most common cause of malignant otitis externa (MOE), which typically affects elderly diabetic patients. Fungi are a rare cause of MOE. MOE can be life-threatening if not recognized and treated promptly. It can result in a wide spectrum of complications, including skull-base osteomyelitis, cranial nerve palsy, cerebral venous thrombosis, and brain abscess. Pseudoaneurysm formation of the intracranial vessels is a life-threatening complication of MOE that is seldom reported in the literature.
Case Report:
We report the case of a 66-year-old diabetic man with MOE who was initially treated with antipseudomonal antibiotics after negative initial culture results. His MOE resulted in a cascade of complications, including facial nerve palsy, skull base osteomyelitis, and sigmoid sinus thrombosis, and culminated in left maxillary artery pseudoaneurysm formation resulting in massive epistaxis and hemodynamic instability. Endovascular embolization resulted in a successful obliteration of the pseudoaneurysm. A subsequent functional endoscopic sinus surgical (FESS) tissue biopsy confirmed Candida glabrata as the etiological agent. The patient was successfully treated with antibiotics and antifungal and anticoagulation therapy, and was discharged home in good condition.
Conclusions:
A high index of suspicion for the diagnosis of fungal MOE, particularly in intractable cases of MOE with negative initial cultures, should be maintained. Pseudoaneurysm formation is a life-threatening complication of MOE that is seldom reported in the literature and should be suspected in any patient with MOE who presents with epistaxis or intracranial bleeding.
Related collections
Most cited references28
- Record: found
- Abstract: found
- Article: not found
Infected (mycotic) aneurysms: spectrum of imaging appearances and management.
- Record: found
- Abstract: found
- Article: not found