- Record: found
- Abstract: found
- Article: found
Lymphatic Drainage Mapping with Indirect Lymphography for Canine Mammary Tumors
Read this article at
Abstract
Simple Summary
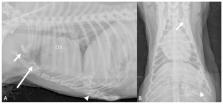
Mammary gland tumours are the most common canine neoplasms. They account for 25–50% of all tumors diagnosed in bitches. Metastases and recurrences develop in about 35–70% of bitches following excision. The presence of regional lymph node metastases is a relevant factor affecting prognosis and treatment in cases of mammary gland tumors. The sentinel lymph node (SLN) is the first lymph node (or nodes) in the regional lymphatic basin that receives lymphatic flow from the primary neoplasm. As mammary gland tumors mainly spread by lymphatic vessels invasion, conceptually, distant metastasis should not be present if the SLN does not have evidence of a tumor burden. In the present study, an indirect lymphography was used for sentinel lymph node mapping in a cohort of 14 adult female dogs with 24 mammary tumors involving the third to the fifth mammary gland. Contrast was injected around the mammary tumor, and lymph nodes that picked up the contrast were visible after 24 h. The results of this study indicate that the lymph drainage pattern of the neoplastic mammary gland may be different for each tumor. The knowledge of the SLN of the neoplastic mammary glands should be of high importance for the surgeon not only for performing the most adequate surgical excision but also for determining an accurate post-surgical prognosis.
Abstract
Mammary gland tumors are the most common canine neoplasms. They account for 25–50% of all tumors diagnosed in bitches. Metastases and recurrences develop in about 35–70% of bitches following excision. The presence of regional lymph node metastases is a relevant factor affecting prognosis and treatment in cases of mammary gland tumors. The sentinel lymph node (SLN) is the first lymph node (or nodes) in the regional lymphatic basin that receives lymphatic flow from the primary neoplasm. The aim of this study is to investigate the SLN with indirect lymphography for a mammary tumor in dogs. The knowledge of the precise drainage pattern and SLN of the neoplastic mammary glands would provide clinically relevant information to the surgeon and to the oncologist, and it would be of high importance for the surgeon not only for performing the most adequate surgical excision but also for determining an accurate post-surgical prognosis.
Related collections
Most cited references39
- Record: found
- Abstract: not found
- Article: not found
Regulation of angiogenesis via vascular endothelial growth factor receptors.
- Record: found
- Abstract: found
- Article: not found
Histopathologic validation of the sentinel lymph node hypothesis for breast carcinoma.
- Record: found
- Abstract: found
- Article: not found