- Record: found
- Abstract: found
- Article: found
Society for Immunotherapy of Cancer (SITC) clinical practice guideline on immunotherapy for the treatment of gynecologic cancer
Read this article at
Abstract
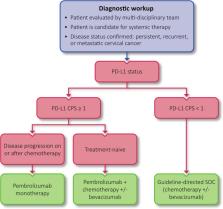
Advanced gynecologic cancers have historically lacked effective treatment options. Recently, immune checkpoint inhibitors (ICIs) have been approved by the US Food and Drug Administration for the treatment of cervical cancer and endometrial cancer, offering durable responses for some patients. In addition, many immunotherapy strategies are under investigation for the treatment of earlier stages of disease or in other gynecologic cancers, such as ovarian cancer and rare gynecologic tumors. While the integration of ICIs into the standard of care has improved outcomes for patients, their use requires a nuanced understanding of biomarker testing, treatment selection, patient selection, response evaluation and surveillance, and patient quality of life considerations, among other topics. To address this need for guidance, the Society for Immunotherapy of Cancer (SITC) convened a multidisciplinary panel of experts to develop a clinical practice guideline. The Expert Panel drew on the published literature as well as their own clinical experience to develop evidence- and consensus-based recommendations to provide guidance to cancer care professionals treating patients with gynecologic cancer.
Related collections
Most cited references299
- Record: found
- Abstract: found
- Article: not found
Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries
- Record: found
- Abstract: found
- Article: not found
Cancer statistics, 2020
- Record: found
- Abstract: found
- Article: not found