- Record: found
- Abstract: found
- Article: found
Value of Hounsfield units measured by chest computed tomography for assessing bone density in the thoracolumbar segment of the thoracic spine
Read this article at
Abstract
Purpose
To investigate the correlation between Hounsfield unit (HU) values measured by chest computed tomography (CT) and dual-energy X-ray absorptiometry (DXA) T-scores. HU-based thoracolumbar (T11 and T12) cutoff thresholds were calculated for a cohort of Chinese patients.
Overview of Literature
For patients with osteoporosis, the incidence of fractures in the thoracolumbar segment is significantly higher than that in other sites. However, most current clinical studies have focused on L1.
Methods
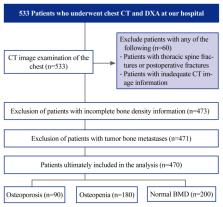
This retrospective study analyzed patients who underwent chest CT and DXA at our hospital between August 2021 and August 2022. Thoracic thoracolumbar segment HU values, lumbar T-scores, and hip T-scores were computed for comparison, and thoracic thoracolumbar segment HU thresholds suggestive of potential bone density abnormalities were established using receiver operating characteristic curves.
Results
In total, 470 patients (72.4% women; mean age, 65.5±12.3 years) were included in this study. DXA revealed that of the 470 patients, 90 (19%) had osteoporosis, 180 (38%) had reduced osteopenia, and 200 (43%) had normal bone mineral density (BMD). To differentiate osteoporosis from osteopenia, the HU threshold was established as 105.1 (sensitivity, 54.4%; specificity, 72.2%) for T11 and 85.7 (sensitivity, 69.4%; specificity, 61.1%) for T12. To differentiate between osteopenia and normal BMD, the HU threshold was 146.7 for T11 (sensitivity, 57.5%; specificity, 84.4%) and 135.7 for T12 (sensitivity, 59.5%; specificity, 80%).
Conclusions
This study supports the significance of HU values from chest CT for BMD assessment. Chest CT provides a new method for clinical opportunistic screening of osteoporosis. When the T11 HU is >146.7 or the T12 HU is >135.7, additional osteoporosis testing is not needed unless a vertebral fracture is detected. If the T11 HU is <105.1 or the T12 HU is <85.7, further DXA testing is strongly advised. In addition, vertebral HU values that fall faster than those of the T11 and L1 vertebrae may explain the high incidence of T12 vertebral fractures.
Related collections
Most cited references34

- Record: found
- Abstract: found
- Article: found
Prevalence of osteoporosis in China: a meta-analysis and systematic review
- Record: found
- Abstract: found
- Article: not found