- Record: found
- Abstract: found
- Article: found
Outcomes of liver transplantation for non-alcoholic steatohepatitis: A European Liver Transplant Registry study

Read this article at
Graphical abstract
Highlights
-
•
An increasing proportion of patients are being transplanted for non-alcoholic steatohepatitis (NASH) in Europe.
-
•
Hepatocellular carcinoma was more common in patients transplanted with NASH.
-
•
Survival in recipients with NASH is comparable to that of other disease indications.
-
•
Age, BMI, and advanced liver disease predicted poorer outcomes in NASH recipients.
Abstract
Background & Aims
Little is known about outcomes of liver transplantation for patients with non-alcoholic steatohepatitis (NASH). We aimed to determine the frequency and outcomes of liver transplantation for patients with NASH in Europe and identify prognostic factors.
Methods
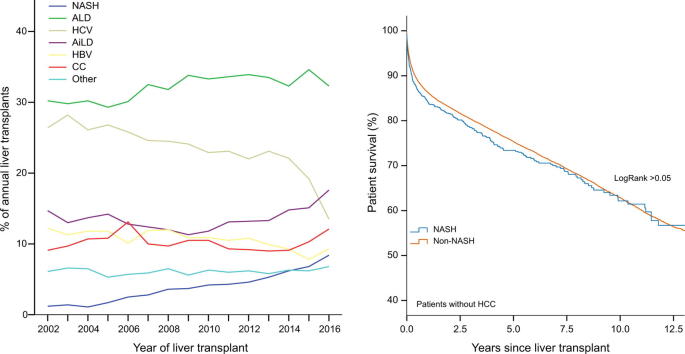
We analysed data from patients transplanted for end-stage liver disease between January 2002 and December 2016 using the European Liver Transplant Registry database. We compared data between patients with NASH versus other aetiologies. The principle endpoints were patient and overall allograft survival.
Results
Among 68,950 adults undergoing first liver transplantation, 4.0% were transplanted for NASH – an increase from 1.2% in 2002 to 8.4% in 2016. A greater proportion of patients transplanted for NASH (39.1%) had hepatocellular carcinoma (HCC) than non-NASH patients (28.9%, p <0.001). NASH was not significantly associated with survival of patients (hazard ratio [HR] 1.02, p = 0.713) or grafts (HR 0.99; p = 0.815) after accounting for available recipient and donor variables. Infection (24.0%) and cardio/cerebrovascular complications (5.3%) were the commonest causes of death in patients with NASH without HCC. Increasing recipient age (61–65 years: HR 2.07, p <0.001; >65: HR 1.72, p = 0.017), elevated model for end-stage liver disease score (>23: HR 1.48, p = 0.048) and low (<18.5 kg/m 2: HR 4.29, p = 0.048) or high (>40 kg/m 2: HR 1.96, p = 0.012) recipient body mass index independently predicted death in patients transplanted for NASH without HCC. Data must be interpreted in the context of absent recognised confounders, such as pre-morbid metabolic risk factors.
Conclusions
The number and proportion of liver transplants performed for NASH in Europe has increased from 2002 through 2016. HCC was more common in patients transplanted with NASH. Survival of patients and grafts in patients with NASH is comparable to that of other disease indications.
Lay summary
The prevalence of non-alcoholic fatty liver disease has increased dramatically in parallel with the worldwide increase in obesity and diabetes. Its progressive form, non-alcoholic steatohepatitis, is a growing indication for liver transplantation in Europe, with good overall outcomes reported. However, careful risk factor assessment is required to maintain favourable post-transplant outcomes in patients with non-alcoholic steatohepatitis.
Related collections
Most cited references19

- Record: found
- Abstract: found
- Article: found
Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants
- Record: found
- Abstract: found
- Article: not found
Projections of primary liver cancer to 2030 in 30 countries worldwide
- Record: found
- Abstract: found
- Article: not found