- Record: found
- Abstract: found
- Article: found
Two-stage revision for prosthetic joint infection: predictors of outcome and the role of reimplantation microbiology
Read this article at
Abstract
Objectives
We describe rates of success for two-stage revision of prosthetic joint infection (PJI), including data on reimplantation microbiology.
Methods
We retrospectively collected data from all the cases of PJI that were managed with two-stage revision over a 4 year period. Patients were managed with an antibiotic-free period before reimplantation, in order to confirm, clinically and microbiologically, that infection was successfully treated.
Results
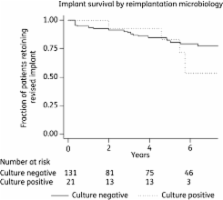
One hundred and fifty-two cases were identified. The overall success rate (i.e. retention of the prosthesis over 5.75 years of follow-up) was 83%, but was 89% for first revisions and 73% for re-revisions [hazard ratio = 2.9, 95% confidence interval (CI) 1.2–7.4, P = 0.023]. Reimplantation microbiology was frequently positive (14%), but did not predict outcome (hazard ratio = 1.3, 95% CI 0.4–3.7, P = 0.6). Furthermore, most unplanned debridements following the first stage were carried out before antibiotics were stopped (25 versus 2 debridements).
Related collections
Most cited references28
- Record: found
- Abstract: found
- Article: not found
The use of the Oxford hip and knee scores.
- Record: found
- Abstract: found
- Article: not found
Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature.
- Record: found
- Abstract: found
- Article: not found