- Record: found
- Abstract: found
- Article: found
Differential diagnosis of amnestic dementia patients based on an FDG-PET signature of autopsy-confirmed LATE-NC
Read this article at
Abstract
Introduction:
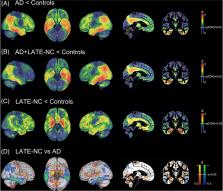
Limbic age-related TDP-43 encephalopathy neuropathologic change (LATE-NC) is common in advanced age and can underlie a clinical presentation mimicking Alzheimer’s disease (AD). We studied whether an autopsy-derived fluorodeoxyglucose positron emission tomography (FDG-PET) signature of LATE-NC provides clinical utility for differential diagnosis of amnestic dementia patients.
Methods:
Ante mortem FDG-PET patterns from autopsy-confirmed LATE-NC ( N = 7) and AD ( N = 23) patients were used to stratify an independent cohort of clinically diagnosed AD dementia patients ( N = 242) based on individual FDG-PET profiles.
Results:
Autopsy-confirmed LATE-NC and AD groups showed markedly distinct temporo-limbic and temporo-parietal FDG-PET patterns, respectively. Clinically diagnosed AD dementia patients showing a LATE-NC–like FDG-PET pattern ( N = 25, 10%) were significantly older, showed less abnormal AD biomarker levels, lower APOE ε4, and higher TMEM106B risk allele load. Clinically, they exhibited a more memory-predominant profile and a generally slower disease course.
Related collections
Most cited references49
- Record: found
- Abstract: found
- Article: found
Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs
- Record: found
- Abstract: found
- Article: not found
National Institute on Aging-Alzheimer's Association guidelines for the neuropathologic assessment of Alzheimer's disease: a practical approach.
- Record: found
- Abstract: found
- Article: not found