- Record: found
- Abstract: found
- Article: found
Minimum 10-Year Clinical Outcomes After Arthroscopic 270° Labral Repair in Traumatic Shoulder Instability Involving Anterior, Inferior, and Posterior Labral Injury
Read this article at
Abstract
Background:
Current literature reports highly satisfactory short- and midterm clinical outcomes in patients with arthroscopic 270° labral tear repairs. However, data remain limited on long-term clinical outcomes and complication and redislocation rates in patients with traumatic shoulder instability involving anterior, inferior, and posterior labral injury.
Purpose:
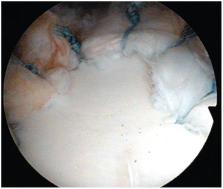
To investigate, at a minimum follow-up of 10 years, the clinical outcomes, complications, and recurrent instability in patients with 270° labral tears involving the anterior, inferior, and posterior labrum treated with arthroscopic stabilization using suture anchors.
Methods:
A retrospective outcomes study was completed for all patients with a minimum 10-year follow-up who underwent arthroscopic 270° labral tear repairs with suture anchors by a single surgeon. Outcome measures included pre- and postoperative Rowe score, American Shoulder and Elbow Surgeons (ASES) score, Simple Shoulder Test, visual analog scale for pain, and Single Assessment Numeric Evaluation (SANE). Western Ontario Shoulder Instability Index (WOSI) scores were collected postoperatively. Complication data were collected, including continued instability, subluxation or dislocation events, and revision surgery. Failure was defined as any cause of revision surgery.
Results:
In total, 21 patients (mean ± SD age, 27.1 ± 9.6 years) with 270° labral repairs were contacted at a minimum 10-year follow-up. All outcome measures showed statistically significant improvements as compared with those preoperatively: Rowe (53.9 ± 11.4 to 88.7 ± 8.9; P = .005), ASES (72.9 ± 18.4 to 91.8 ± 10.8; P = .004), Simple Shoulder Test (8.7 ± 2.4 to 11.2 ± 1.0; P = .013), visual analog scale (2.5 ± 2.6 to 0.5 ± 1.1; P = .037), and SANE (24.0 ± 15.2 to 91.5 ± 8.3; P = .043). The mean postoperative WOSI score at minimum follow-up was 256.3 ± 220.6. Three patients had postoperative complications, including a traumatic subluxation, continued instability, and a traumatic dislocation, 2 of which required revision surgery (14.2% failure rate).
Conclusion:
Arthroscopic repairs of 270° labral tears involving the anterior, inferior, and posterior labrum have highly satisfactory clinical outcomes at 10 years, with complication and redislocation rates similar to those reported at 2 years. This suggests that repairs of extensile labral tears are effective in restoring and maintaining mechanical stability of the glenohumeral joint in the long term.
Related collections
Most cited references22
- Record: found
- Abstract: found
- Article: not found
Inferior capsular shift for involuntary inferior and multidirectional instability of the shoulder. A preliminary report.

- Record: found
- Abstract: found
- Article: found
The Western Ontario Shoulder Instability Index (WOSI): validity, reliability, and responsiveness retested with a Swedish translation
- Record: found
- Abstract: found
- Article: not found