- Record: found
- Abstract: found
- Article: found
RISK FACTORS FOR SEVERE POSTOPERATIVE COMPLICATIONS AFTER GASTRECTOMY FOR GASTRIC AND ESOPHAGOGASTRIC JUNCTION CANCERS Translated title: FATORES DE RISCO PARA COMPLICAÇÕES PÓS-OPERATÓRIAS GRAVES APÓS GASTRECTOMIA POR CÂNCER DO ESTÔMAGO E JUNÇÃO ESOFAGOGÁSTRICA
ABSTRACT
Background:
Gastrectomy is the main treatment for gastric and Siewert type II-III esophagogastric junction (EGJ) cancer. This surgery is associated with significant morbidity. Total morbidity rates vary across different studies and few have evaluated postoperative morbidity according to complication severity.
Methods:
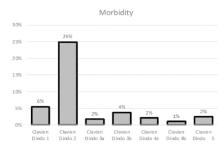
This was a retrospective cohort study from a prospective database. We included patients treated with gastrectomy for gastric or EGJ cancers between January 2012 and December 2016 at a single center. Severe morbidity was defined as Clavien-Dindo score ≥3. A multivariate analysis was performed to identify predictors of severe morbidity.
Results:
Two hundred and eighty-nine gastrectomies were performed (67% males, median age: 65 years). Tumor location was EGJ in 14%, upper third of the stomach in 30%, middle third in 26%, and lower third in 28%. In 196 (67%), a total gastrectomy was performed with a D2 lymph node dissection in 85%. Two hundred and eleven patients (79%) underwent an open gastrectomy. T status was T1 in 23% and T3/T4 in 68%. Postoperative mortality was 2.4% and morbidity rate was 41%. Severe morbidity was 11% and was mainly represented by esophagojejunostomy leak (2.4%), duodenal stump leak (2.1%), and respiratory complications (2%). On multivariate analysis, EGJ location and T3/T4 tumors were associated with a higher rate of severe postoperative morbidity.
RESUMO
l: A gastrectomia é o tratamento principal para o câncer de junção esofagogástrica (EGJ) e Siewert tipo II-III. Ela está associada à morbidade significativa. As taxas de morbidade total variam entre os diferentes estudos e poucos avaliaram a morbidade pós-operatória de acordo com a gravidade da complicação.
Este foi um estudo de coorte retrospectivo de um banco de dados prospectivo. Foram incluídos pacientes tratados com gastrectomia para câncer gástrico ou EGJ em um único centro. A morbidade severa foi definida como escore de Clavien-Dindo ≥3. Análise multivariada foi realizada para identificar preditores de morbidade grave.
Duzentos e oitenta e nove gastrectomias foram realizadas (67% homens, mediana de idade: 65 anos). A localização do tumor foi EGJ em 14%, o terço superior do estômago em 30%, o terço médio em 26% e o terço inferior em 28%. Em 196 (67%), foi realizada gastrectomia total com dissecção de linfonodos D2 em 85%. Duzentos e onze pacientes (79%) foram submetidos à gastrectomia aberta. O estado T foi T1 em 23% e T3/T4 em 68%. A mortalidade pós-operatória foi de 2,4% e a taxa de morbidade foi de 41%. A morbidade severa foi de 11% e foi representada principalmente por fístula esofagojejunal (2,4%), fístula duodenal (2,1%) e complicações respiratórias (2%). Na análise multivariada, a localização do EGJ e os tumores T3/T4 foram associados com maior morbidade pós-operatória grave.
Related collections
Most cited references25
- Record: found
- Abstract: not found
- Article: not found
Classification of adenocarcinoma of the oesophagogastric junction.
- Record: found
- Abstract: found
- Article: not found
Decreased Morbidity of Laparoscopic Distal Gastrectomy Compared With Open Distal Gastrectomy for Stage I Gastric Cancer: Short-term Outcomes From a Multicenter Randomized Controlled Trial (KLASS-01).
- Record: found
- Abstract: found
- Article: not found