- Record: found
- Abstract: found
- Article: found
Prognosis Evaluation of MRI Combined with Magnetic Resonance Myelography on Lumbar Disc Herniation after Transforaminal Endoscopic Discectomy
Read this article at
Abstract
Objective
This study sets out to investigate the role of magnetic resonance imaging (MRI) combined with magnetic resonance myelography (MRM) in patients after percutaneous transforaminal endoscopic discectomy (PTED) and to evaluate its value in postoperative rehabilitation.
Methods
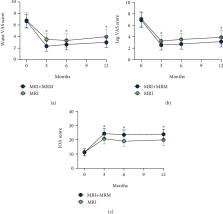
The clinical date of 96 patients with lumbar disc herniation (LDH) after PTED was retrospectively analyzed. The enrolled patients were divided into MRI group ( n = 32) and MRI + MRM group ( n = 64) according to whether MRM was performed. The nerve root sleeve (morphology, deformation) and dural indentation, intervertebral space height (ISH), intervertebral space angle (ISA), degree of pain (Visual Analogue Scale (VAS)), vertebral function (Japanese Orthopaedic Association (JOA)), and long-term recurrence were compared between the two groups.
Results
Compared with the MRI group, the MRI + MRM group better displayed nerve root morphology, sheath sleeve deformation, and dural indentation. Both MRI and MRI + MRM showed ISH and ISA changes well. Compared with the MRI group, the MRI + MRM group had a significantly lower VAS score for lumbar and leg pain, a significantly higher JOA score, and a significantly lower 2-year recurrence rate.
Related collections
Most cited references32
- Record: found
- Abstract: found
- Article: not found
Measurement Properties of Visual Analogue Scale, Numeric Rating Scale, and Pain Severity Subscale of the Brief Pain Inventory in Patients With Low Back Pain: A Systematic Review
- Record: found
- Abstract: found
- Article: not found
Comparison of percutaneous endoscopic transforaminal discectomy, microendoscopic discectomy, and microdiscectomy for symptomatic lumbar disc herniation: minimum 2-year follow-up results
- Record: found
- Abstract: found
- Article: not found