- Record: found
- Abstract: found
- Article: found
Quality of life questionnaire predicts poor exercise capacity only in HFpEF and not in HFrEF
Read this article at
Abstract
Background
The Minnesota Living with Heart Failure Questionnaire (MLHFQ) is the most widely used measure of quality of life (QoL) in HF patients. This prospective study aimed to assess the relationship between QoL and exercise capacity in HF patients.
Methods
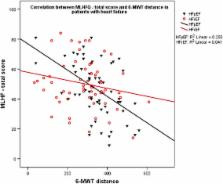
The study subjects were 118 consecutive patients with chronic HF (62 ± 10 years, 57 females, in NYHA I-III). Patients answered a MLHFQ questionnaire in the same day of complete clinical, biochemical and echocardiographic assessment. They also underwent a 5 min walk test (6-MWT), in the same day, which grouped them into; Group I: ≤ 300 m and Group II: >300 m. In addition, left ventricular (LV) ejection fraction (EF), divided them into: Group A, with preserved EF (HFpEF) and Group B with reduced EF (HFrEF).
Results
The mean MLHFQ total scale score was 48 (±17). The total scale, and the physical and emotional functional MLHFQ scores did not differ between HFpEF and HFpEF. Group I patients were older ( p = 0.003), had higher NYHA functional class ( p = 0.002), faster baseline heart rate ( p = 0.006), higher prevalence of smoking ( p = 0.015), higher global, physical and emotional MLHFQ scores ( p < 0.001, for all), larger left atrial (LA) diameter ( p = 0.001), shorter LV filling time ( p = 0.027), higher E/e’ ratio (0.02), shorter isovolumic relaxation time ( p = 0.028), lower septal a’ ( p = 0.019) and s’ ( p = 0.023), compared to Group II.
Independent predictors of 6-MWT distance for the group as a whole were increased MLHFQ total score ( p = 0.005), older age ( p = 0.035), and diabetes ( p = 0.045), in HFpEF were total MLHFQ ( p = 0.007) and diabetes (p = 0.045) but in HFrEF were only LA enlargement (p = 0.005) and age ( p = 0.013. A total MLHFQ score of 48.5 had a sensitivity of 67% and specificity of 63% (AUC on ROC analysis of 72%) for limited exercise performance in HF patients.
Related collections
Most cited references44
- Record: found
- Abstract: found
- Article: not found
Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings.
- Record: found
- Abstract: found
- Article: not found
The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure.
- Record: found
- Abstract: found
- Article: not found