- Record: found
- Abstract: found
- Article: found
Timing, causes, predictors and prognosis of switching from peritoneal dialysis to hemodialysis: a prospective study
Read this article at
Abstract
Background
The use of peritoneal dialysis (PD) has declined in the United States over the past decade and technique failure is also reportedly higher in PD compared to hemodialysis (HD), but there are little data in the United States addressing the factors and outcomes associated with switching modalities from PD to HD.
Methods
In a prospective cohort study of 262 PD patients enrolled from 28 peritoneal dialysis clinics in 13 U.S. states, we examined potential predictors of switching from PD to HD (including demographics, clinical factors, and laboratory values) and the association of switching with mortality. Cox proportional hazards regression was used to assess relative hazards (RH) of switching and of mortality in PD patients who switched to HD.
Results
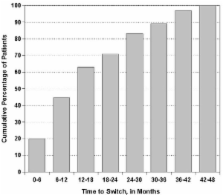
Among 262 PD patients, 24.8% switched to HD; with more than 70% switching within the first 2 years. Infectious peritonitis was the leading cause of switching. Patients of black race and with higher body mass index were significantly more likely to switch from PD to HD, RH (95% CI) of 5.01 (1.15–21.8) for black versus white and 1.09 (1.03–1.16) per 1 kg/m 2 increase in BMI, respectively. There was no difference in survival between switchers and non-switchers, RH (95% CI) of 0.89 (0.41–1.93).
Conclusion
Switching from PD to HD occurs early and the rate is high, threatening long-term viability of PD programs. Several patient characteristics were associated with the risk of switching. However, there was no survival difference between switchers and non-switchers, reassuring providers and patients that PD technique failure is not necessarily associated with poor prognosis.
Related collections
Most cited references38
- Record: found
- Abstract: found
- Article: not found
Effects of increased peritoneal clearances on mortality rates in peritoneal dialysis: ADEMEX, a prospective, randomized, controlled trial.
- Record: found
- Abstract: found
- Article: not found
The timing of specialist evaluation in chronic kidney disease and mortality.
- Record: found
- Abstract: found
- Article: not found